Not all crown & bridge labs are prepared to meet the diverse demands of today’s clinical workflows and patient preferences.
Labs limited to a narrow material range or lacking documentation often force clinics into compromises—either on esthetics, budget, or safety.
By evaluating material variety, digital compatibility, clinical adaptability, and sourcing transparency, you can partner with a lab that enhances both treatment flexibility and operational confidence.
A dental lab should provide a full range of crown and bridge materials, including full-contour and layered zirconia, lithium disilicate, PFM, hybrid ceramics, and metal alloys like nickel‑chromium or cobalt‑chromium. It should support digital workflow compatibility, offer tiered pricing structures, and supply documentation such as batch numbers, CE/FDA certificates, and biocompatibility reports.
What are the core material categories for crown & bridge restorations?
Crown & bridge labs must offer a complete material portfolio to serve the full range of clinical indications. From strength-demanding posterior units to esthetic anterior veneers, having access to multiple materials allows dentists to choose restorations based on both function and appearance.

Dental-Crown-Bridge-Materials-Zirconia-PFM-LithiumDisilicate
Common types: metal alloys, full-contour zirconia, layered zirconia, lithium disilicate, PFM, hybrid materials
Modern labs typically stock:
- Full-contour zirconia: high strength, ideal for posterior
- Layered zirconia: esthetic anterior cases needing translucency
- Lithium disilicate (e.g. E.max): esthetics-focused for veneers, inlays
- PFM (porcelain-fused-to-metal): durable and cost-effective in mixed restorations
- Non-precious/precious metal alloys: for metal-ceramic bridges or full-cast units
- Hybrid materials: like composite-ceramic mixes for temporaries
A broad material base ensures readiness for different case types.
Pros & cons of monolithic vs. layered restorations
Material form impacts strength, esthetics, and price.
| Type | Strength | Esthetics | Use Case | Notes |
|---|---|---|---|---|
| Monolithic zirconia | ★★★★★ | ★★☆☆☆ | Posterior | Low wear, opaque |
| Layered zirconia | ★★★★☆ | ★★★★☆ | Anterior | Balanced, more lifelike |
| Lithium disilicate | ★★★☆☆ | ★★★★★ | Veneers/Inlays | Best esthetics, fragile in bridges |
Choosing the right type depends on indication—not just preference.
Why offering complete material range ensures lab responsiveness
When a lab stocks and works with a complete material spectrum:
- No delay in ordering special materials for less common indications
- Faster adaptation to evolving clinical preferences or technology
- Better support for mixed-arch or full-mouth cases
- Stronger collaboration with clinics using indication-specific protocols
Material flexibility means clinical agility—and higher lab reliability.
✅ A full material range enables better case adaptation and client fit – TRUE
Clinicians can match indication to the best-performing material without workflow disruption.
❌ Zirconia alone covers all crown & bridge needs – FALSE
While versatile, zirconia lacks the esthetic nuance or flexibility needed for many anterior or hybrid applications.
How do material choices align with different clinical scenarios?
Not all materials suit every case. A crown & bridge lab must understand which materials best fit specific clinical scenarios—balancing strength, esthetics, and case complexity—to support better treatment outcomes and reduce adjustments or remakes.

Dental-Crown-Material-Clinical-Scenario-Matching
Material suitability for anterior vs. posterior cases
The restoration zone determines key material priorities:
- Anterior restorations: focus on translucency and shade blending
- Preferred: layered zirconia, lithium disilicate
- Posterior crowns or bridges: prioritize strength and longevity
- Preferred: full-contour zirconia, PFM
- Aesthetic zones with functional load: balance needed
- Preferred: high-translucency zirconia or reinforced lithium disilicate
Material selection here is about visibility, loading, and patient esthetic demand.
Options for implants, veneers, and long-span bridges
Different indications come with distinct material needs:
- Implant-supported restorations
- Full-contour zirconia for strength + tissue tolerance
- PFM when retrievability or metal collar is preferred
- Veneers or partial crowns
- Lithium disilicate or hybrid ceramics for thin, bonded applications
- Long-span bridges
- Monolithic zirconia for rigidity, PFM if large connectors are needed
Choosing based on clinical indication reduces technical compromise later.
Balancing esthetic, strength, and complexity requirements
Some cases require hybrid decision-making between beauty, strength, and risk.
- High esthetic demand + low bite force → lithium disilicate
- Moderate esthetics + high function → layered zirconia or HT zirconia
- Challenging prep or occlusion cases → PFM or full-zirconia for resilience
- Mixed-arch or full-mouth rehab → combine materials based on arch zone
Good labs help clients find the right compromise—not just default to one material.
A material is only ideal when it suits both the clinical and functional needs of the case. Contact us for our clinical indication–material pairing chart to plan your next case with more clarity.
What material tiers support varied budget structures?
Crown & bridge labs that serve diverse clients—from private clinics to DSOs—must offer tiered material options. This enables clients to select restorations that fit clinical needs and patient budgets without compromising safety or reliability.

Dental-Crown-Material-Tier-Cost-Comparison
Cost comparison: gold/alloys vs. zirconia vs. lithium disilicate
Each material comes with a distinct cost profile:
| Material | Estimated Cost Tier | Strength | Esthetics | Common Use |
|---|---|---|---|---|
| Gold or precious alloys | $$$ (high) | ★★★★☆ | ★★☆☆☆ | Full-cast crowns, PFM |
| Lithium disilicate (E.max) | $$ (medium) | ★★★☆☆ | ★★★★★ | Veneers, anterior crowns |
| Full-contour zirconia | $ (value) | ★★★★★ | ★★★☆☆ | Posterior units, bridges |
This comparison helps dentists balance case needs with budget sensitivity.
When is PFZ or full-contour zirconia a cost-effective choice?
Some restorations combine esthetics with budget efficiency.
- PFZ (Porcelain-Fused-to-Zirconia)
- Combines translucent base with ceramic layering
- Suitable for anterior cases with moderate budget
- Full-contour zirconia
- Durable and fast to fabricate
- Ideal for large orders or posterior bulk cases
- Stain-glazed monolithic zirconia
- Low-cost esthetic compromise for less visible zones
These options help clinics avoid costly upgrades when not clinically needed.
Tiered materials strategy for labs working with diverse client budgets
Tiering supports flexibility across client types and regions:
- High-tier: gold-based PFM or multilayer zirconia for premium patients
- Mid-tier: E.max, PFZ, or layered zirconia for esthetic-conscious zones
- Entry-tier: monolithic zirconia or PMMA temporaries for limited-budget cases
- Adjustable offerings: labs can scale by volume discounts or material swaps
Smart labs don’t just offer one material—they offer structure.
✅ Tiered material options enable cost alignment without compromising safety – TRUE
With proper planning, labs can help clients meet budget needs using clinically sound materials.
❌ Lower-priced materials always mean lower quality – FALSE
Many modern materials like full-contour zirconia offer excellent performance at accessible pricing.
How should a lab ensure digital workflow compatibility across materials?
Material-specific design parameters must be integrated into the digital workflow for a crown & bridge lab to deliver accurate, consistent results. Each material—zirconia, lithium disilicate, PFM—has its own requirements for thickness, margin, and process type. Labs that pre-calibrate their CAD and milling settings help reduce chairside adjustments and remakes, as shown in a systematic review on digital vs conventional workflows that emphasizes precision and consistency across material-specific settings.
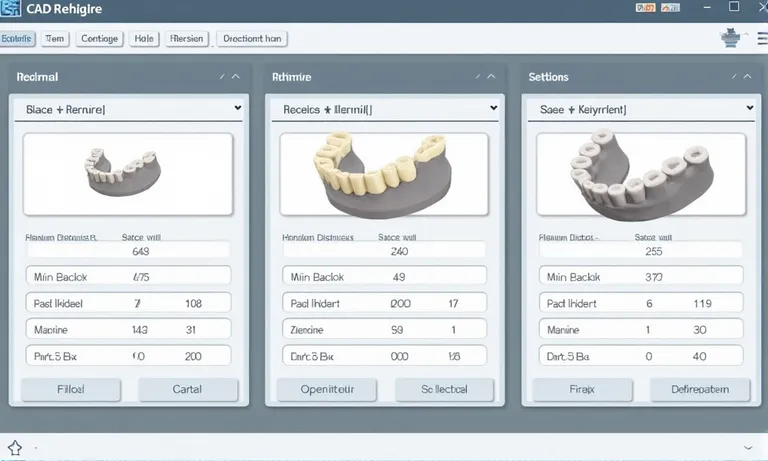
CAD-Material-Settings-Dental-Lab-Zirconia-Lithium-PFM
STL carving, margin design, and minimum thickness by material type
Each material has its own design thresholds:
- Full-contour zirconia
- Minimum thickness: ~0.7 mm
- Ideal for knife-edge or chamfer preps
- Lithium disilicate (E.max)
- Minimum thickness: ~1.0–1.5 mm
- Needs uniform reduction for esthetics
- PFM frameworks
- Minimum metal coping: ~0.5 mm + ceramic layering
- Requires controlled space for metal and ceramic
Applying the correct parameters in CAD ensures proper strength and fit.
CAD parameters: milling vs. pressing vs. layering processes
Labs must adjust design strategy based on restoration type and processing method:
- Milled zirconia: shrinkage compensation built into CAM
- Pressed lithium disilicate: requires wax-up or digital mold printing
- Layered restorations: core must support esthetic build-up, especially at incisal edge
Wrong design workflows increase fracture risk and reduce long-term survival.
Scanner and design system compatibility per material
Material planning must align with scanner output and design platform settings:
- Exocad and 3Shape: preset libraries for major materials
- iOS scans: higher resolution supports tight margin definitions
- Cross-platform STL imports: lab must test fit tolerance per material on each system
- Cloud-based workflows: benefit from pre-loaded parameters synced across cases
Labs familiar with this integration reduce need for chairside adjustments.
Digital workflows are only effective if aligned with each material’s structural and esthetic requirements. Proper calibration at every step—design, scan, and CAM—ensures your restorations arrive functional and predictable.
What compliance documentation and material sourcing transparency should be needed?
Labs must be able to demonstrate that all materials used in crown & bridge restorations are safe, traceable, and approved for dental use. Clear documentation builds trust with clients and regulators—especially when cases cross international borders.

Image
ALT: Dental-Material-Compliance-Documentation-Batch-Labels
Prompt:
A highly realistic, ultra-detailed, professional-quality image showing dental lab compliance documents neatly arranged on a clean countertop: including batch number labels, certificates of origin, FDA/CE certificates, and SDS (Safety Data Sheets). A technician’s gloved hand is organizing the files. Soft daylight highlights the details and clarity.
Material batch numbers, certificates of origin, and raw material audit trails
Every material should be fully traceable:
- Batch numbers: labeled on internal production logs and cases
- Certificates of origin: verify where zirconia, metal, or ceramic is sourced
- Audit trails: show storage conditions, expiration, and lot handling
Traceability protects both the clinic and patient in case of quality disputes.
FDA/CE/ISO approval standards for dental materials
Regulatory documents should be aligned with export market:
- FDA 510(k) or Custom Device Exemption for U.S.
- CE Class IIa Declaration of Conformity for EU markets
- ISO 10993 / ISO 13485 evidence for internal QA system alignment
- Third-party verification from certified bodies preferred
Clients should confirm these certificates are valid and matched to the correct product type.
Biocompatibility reports and safety data sheet availability
Labs should provide supporting material safety documentation:
- Biocompatibility test summaries for materials in direct oral contact
- Safety Data Sheets (SDS) for zirconia, e.max, alloys, etc.
- Radiopacity and wear index data for product-specific selection
- Lab-internal material usage logs for case-by-case reference
This transparency supports compliance in audits, tenders, and recordkeeping.
Reliable labs integrate compliance into their daily workflow—not just during inspections. Request our material audit pack to verify every crown & bridge restoration meets international safety and documentation standards.
Conclusion
Crown & bridge material capability is more than a product list—it’s a reflection of how well a dental lab can support case diversity, patient expectations, and regulatory responsibility. Labs that offer material flexibility, digital readiness, and documentation transparency position their clients for both clinical precision and operational scale.
- A reliable dental lab delivers a complete spectrum of crown & bridge materials tailored to different indications, aesthetics, and strength requirements.
- Each case type benefits from clinically appropriate materials matched to anatomical and functional needs, reducing adjustment time and risk. clinically appropriate materials matched to anatomical and functional needs
- A lab that supports tiered material pricing structures for various patient budgets enables clinics to serve more patients without compromising quality. tiered material pricing structures for various patient budgets
- Seamless digital workflows depend on material-calibrated CAD/CAM settings and scanner integration to ensure restoration predictability. material-calibrated CAD/CAM settings and scanner integration
- A mature lab should maintain clear documentation of material origin, approval status, and safety compliance for every case delivered. clear documentation of material origin, approval status, and safety compliance
- Supporting clinical quality also means having verifiable technician training and SOP records to ensure materials are processed accurately. verifiable technician training and SOP records
To explore how Raytops Dental Lab aligns material variety with digital design and regulatory fit, contact our case coordination team here.