Implant-supported and posterior bridges present some of the highest technical demands in restorative dentistry—missteps in design or production can lead to fractures, screw loosening, or full remakes.
Yet many labs overlook the extra precision, engineering, and quality control needed to handle these restorations reliably at scale.
By evaluating CAD expertise, occlusal management, digital workflow readiness, and remake safeguards, clinics can confidently choose a lab partner ready for high-complexity bridge cases.
To assess a dental lab’s fit for implant-supported or posterior bridges, evaluate its experience with long-span and implant-splinted restorations, passive fit protocols, connector design proficiency, and full-arch CAD workflows. Also check their ability to translate digital scans accurately, their remake policy, and their fit-testing and adjustment procedures.
What technical capabilities are essential for implant-supported and posterior bridge cases?
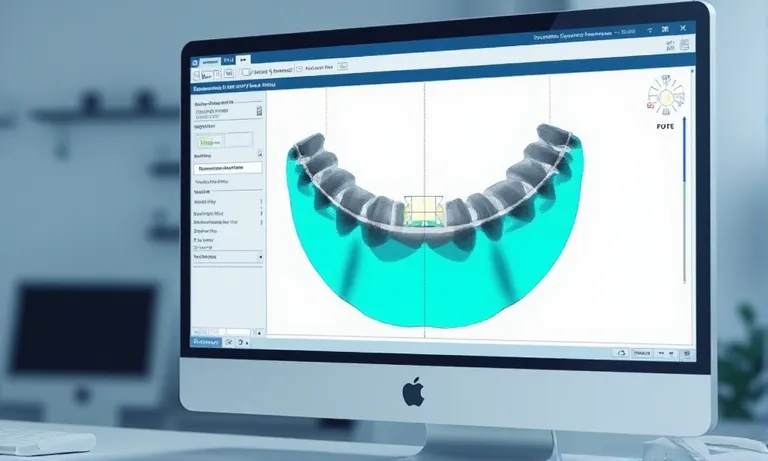
Implant-supported and posterior bridges require advanced technical capabilities due to high bite forces, alignment sensitivity, and screw-access design. Labs must demonstrate a firm grasp of passive fit, biomechanical planning, and connector optimization to ensure long-term restoration stability—especially when dealing with multi-unit prostheses. Studies have shown that achieving true passive fit in screw-retained implant superstructures significantly reduces mechanical complications such as screw loosening and framework fractures.
CAD-Implant-Bridge-Design-Screw-Passive-Fit-Connector
Key design challenges: passive fit, connector stress, screw channel access
Implant and posterior bridges pose several precision challenges:
- Passive fit: Must prevent tension on implants or screws
- Connector zones: Require specific dimensions to withstand load
- Screw channel access: Must be angled without compromising structure
- Emergence profile: Demands soft tissue compatibility and hygiene-friendly shape
- Insertion path: Complex arch forms need precise multi-unit path planning
Missing any of these can result in fractures or biologic complications.
Why implant and posterior bridges require higher technician precision
These restorations go beyond standard crown design:
- Higher load-bearing zone: Back teeth endure stronger occlusal forces
- More rigid support: Implants don’t move like natural teeth—tension accumulates
- Multi-unit synchrony: All retainers must seat simultaneously and equally
- Narrow error margin: Minor CAD or milling inaccuracy leads to clinical misfit
Technician error in this context leads to screw loosening, prosthetic failure, or patient discomfort.
Lab’s role in managing biomechanical risks and restoration stability
An experienced lab anticipates and engineers for clinical longevity:
- Stress distribution: Designs with occlusal guards and compensatory features
- Connector engineering: Calibrated thickness, cross-section, and placement
- Screw channel design: Adjusted for strength and aesthetic masking
- Framework support: Consideration of span length, cantilever presence, and reinforcement zones
Good design is invisible when it works—but crucial when it doesn’t.
✅ Implant-supported bridges require specialized design to avoid biomechanical failure – TRUE
Labs must manage connector thickness, insertion path, and passive fit to ensure long-term function.
❌ Any lab with crown experience can deliver complex bridge restorations – FALSE
Without bridge-specific CAD skills and load planning experience, errors often lead to costly remakes.
How to evaluate a lab’s experience with high-complexity restorations?
A lab’s true capability in implant-supported or posterior bridge cases is best measured through its documented experience. Requesting actual case portfolios, remake metrics, and consistency records gives you insight into how well the lab performs under complex demands—not just what they claim.

Dental-Lab-Bridge-Portfolio-Remake-Analysis
What case types has the lab delivered? Ask for bridge portfolios
Reviewing case samples reveals actual execution depth:
- Long-span posterior bridges: 4+ unit restorations across molars
- Implant-splinted bridges: screw-retained cases with emergence profile control
- Anterior implant bridges: esthetic zones requiring layering and margin masking
- Cantilevered structures: proof of biomechanical judgment
Don’t rely on general product brochures—request categorized examples.
Interpreting remake records and consistency data
Remake and QC metrics reflect real-world performance:
- Remake percentage by bridge type: below 3% for implant bridges is a strong indicator
- Root cause breakdowns: reveals handling of passive fit, margin, occlusion errors
- Consistency over time: monthly or quarterly remake trendlines
- Resolution timeline logs: how fast and clearly issues were addressed
Mature labs track and share these figures as part of QA transparency.
Red flags in long-span or implant-splinted restoration outcomes
Look out for patterns that suggest inexperience:
- Frequent remake due to seating issues or screw loosening
- Inconsistent emergence profiles between abutments
- Fracture in connector zones with no design adjustment history
- Missing support documentation on complex bridge logic
Even a lab with good single-unit delivery may struggle with full-arch or splinted designs.
A capable lab is proud to show how it handles complex cases—and ready to share real data. Request sample bridge portfolios and remake statistics to verify technical experience before committing to high-value cases.
What digital workflow capabilities should the lab demonstrate?
To successfully deliver implant-supported or posterior bridge restorations, a lab must manage complex digital workflows from scan intake to final design. Platform compatibility, file calibration, and scanbody protocols directly impact fit, esthetics, and chairside efficiency.

Full-Arch-Digital-Workflow-Dental-Lab-STL-Scanbody
Full-arch CAD protocols and scan body integration
A qualified lab follows a structured digital flow for full-arch restorations:
- Receive STL scans with scanbody clearly captured
- Identify and segment scanbodies by platform (e.g., Straumann, Nobel)
- Define arch curve and occlusal plane alignment
- Evaluate insertion path for each unit and collective span
- Initiate framework design with screw channel planning
- Simulate seating and verify passive fit digitally
Each step prevents tension buildup and misfit during final placement.
STL parameter control: emergence profile, path of insertion, margin control
Digital success relies on controlling fine STL variables:
- Emergence profile: tailored to soft tissue contours
- Path of insertion: single vs. multi-unit calibration to ensure alignment
- Margin depth and design: especially critical around implant interfaces
- Spacer and cement gap: set per material and platform
- Connector zone sculpting: defined digitally for stress tolerance
Labs that manually adjust STL input ensure better results than fully automated workflows.
Platform compatibility: 3Shape, Exocad, Medit workflows
The lab’s design system must match your scan source:
- 3Shape: scanbody libraries, bridge design presets
- Exocad: open STL flow, compatible with most IO scans
- Medit: accurate soft tissue capture, requires lab-side calibration
- Cross-platform STL clean-up: lab must normalize files to avoid stitching issues
- Cloud system syncing: helpful for multi-stage full-arch cases
Without this compatibility, even well-scanned cases can result in flawed outcomes.
Digitally enabled labs don’t just “receive files”—they optimize, verify, and correct STL data to fit each implant or bridge indication.
How does the lab manage occlusion, connectors, and long-span stability?
In full-arch or posterior bridge cases, occlusal forces are intense and misalignment risks are high. Labs must actively engineer each design to manage articulation, connector strength, and distal extension—otherwise long-term stability is compromised.
Bridge-Design-Occlusion-Connector-Stability-Dental-Lab
Occlusal adjustment strategy and articulation protocols
Proper occlusion handling prevents fractures and seating issues:
- Virtual articulation: Used in CAD for occlusal simulation
- Disclusion rules: No posterior contact in lateral excursions
- Occlusal contact tuning: Prioritized on implant vs. natural tooth cases
- Balanced occlusion: Ensures even distribution on long spans
- Manual verification: Cases adjusted based on model articulation
Labs that skip these steps risk high chairside adjustment or fracture.
Minimum connector size and shape by bridge span
Connector integrity is vital in resisting functional load:
- Posterior bridges: ≥4 mm height, ≥3 mm width recommended
- Long-span bridges: Increase cross-sectional thickness for rigidity
- Anatomic connector design: Rounded transitions reduce stress
- Cantilevered zones: Reinforced with thicker connectors or metal substructure
Undersized or misaligned connectors are top causes of mid-span failure.
Distal extension control and reinforcement methods
Poorly controlled extensions stress implants and material:
- Limit cantilever to 1.5–2 units beyond last support
- Reinforced framework: Zirconia core thickening or metal bar integration
- Tissue support design: Smooth emergence profile for hygiene access
- Case-by-case adjustment: Based on opposing occlusion and span width
Failure to reinforce long spans leads to screw loosening or ceramic fracture.
✅ Bridge connector design directly affects restoration longevity – TRUE
Connector size, shape, and placement must be planned based on span length and occlusal load.
❌ All bridge frameworks can follow a standard connector size – FALSE
Each case requires customized engineering based on span, material, and biomechanical demands.
What QA and remake safeguards does the lab offer for complex bridge cases?
To successfully deliver high‑complexity restorations like implant‑supported or long‑span bridges require additional QA checkpoints and remake protocols to ensure delivery consistency. Labs must embed verification loops, clinical feedback channels, and clear remake accountability into their operations.
Dental-Bridge-QA-Remake-Process-Diagram
Pre-production technical review checkpoints
- Case intake QC: File validation, implant details, opposing model presence
- CAD design review: Passive fit, connector dimensions, screw path clearance
- Framework milling check: Verify material integrity, no voids or distortion
- Final contour inspection: Ensure margin seal and occlusal contacts
- Packaging QC: Labeling, screw inclusion, and delivery checklist
Each step adds confidence before dispatch, especially in multi-unit restorations.
Feedback and adjustment loop with clinics
Effective labs maintain open correction channels:
- Clinic-side observations: Seating resistance, occlusal points, contact tightness
- Photographic returns: Help pinpoint passive fit or angulation issues
- Case history linking: Adjustments fed back into lab software for future remakes
- Technical discussion loop: Shared screenshots or markup files for solution review
This reduces repeated errors and strengthens long-term alignment.
Handling remakes for long-span or implant-supported work
Remakes for complex cases require structure, not improvisation:
- Root cause analysis: Confirm if design, production, or file issue
- Prioritize remake timelines: Especially for chairside delays or urgent delivery
- No-blame adjustments: Focused on restoring trust, not blame
- Logged resolution record: For traceability in future interactions
Bridge remakes are expensive—an organized policy saves both time and confidence.
Experienced labs don’t just “correct mistakes”—they build structured systems to prevent them. Request our complex bridge QA protocol and remake policy to understand how Raytops ensures predictable outcomes and professional support.
Conclusion
Labs that support implant-supported and posterior bridges must go beyond basic delivery—they must demonstrate engineering-level design thinking, digital fluency, and structured QA protocols. Evaluating these capabilities helps clinics reduce remake risk and deliver long-span restorations that stand the test of time.
- A capable lab ensures precision design and biomechanical planning for complex bridge cases, especially those involving implants or posterior load zones.
- Before committing to a supplier, check whether they have verified experience in long-span and implant-splinted restorations with documented results. verified experience in long-span and implant-splinted restorations
- Labs should demonstrate full digital workflow integration with scanbody libraries and STL parameter control for implant platforms. digital workflow integration with scanbody libraries and STL parameter control
- Long-term bridge durability depends on the lab’s expertise in occlusion handling, connector strength, and span-specific reinforcement. occlusion handling, connector strength, and span-specific reinforcement
- For high-value cases, labs must apply structured QA reviews and proactive remake policies to maintain consistency and clinician confidence. structured QA reviews and proactive remake policies
- Choosing the right lab means confirming its technical systems for passive fit, screw access, and connector optimization are already in place. technical systems for passive fit, screw access, and connector optimization
Want to assess if Raytops is technically equipped for your next implant or full-arch bridge case? Contact our team to review technical workflows and sample case protocols.