Complex dental implant restorations are not only clinical challenges but also decisive factors in selecting the right lab partner. Full arch reconstructions, All-on-4 frameworks, and screw-retained hybrids demand far more than basic production capacity. For buyers, success depends less on cost or location and more on whether a lab can deliver precision, digital integration, and consistent reliability in high-stakes cases.
Procurement teams should evaluate several critical areas before committing:
- Case Experience Fit – proven delivery of full arch, All-on-4, or multi-unit restorations.
- Technical Capabilities – use of CAD/CAM systems, digital planning tools like exocad or 3Shape, and custom abutment handling.
- Material Handling – expertise with zirconia, titanium, and hybrid frameworks that ensure biocompatibility.
- Communication Protocols – structured feedback loops, virtual previews, and case design verification.
- Quality Assurance – remake rate control, QC checkpoints, and consistency across production.
- Delivery Alignment – realistic lead times and transparent capacity for multi-case scheduling.
Choosing a lab for complex implant cases is less about finding a vendor and more about building a partnership with a proven, workflow-aligned overseas dental lab. This collaboration transforms complexity into predictable outcomes, safeguarding both clinic schedules and patient satisfaction.
How Product Complexity Impacts Dental Lab Selection
Complex implant cases require different decision criteria compared with single-unit crowns or simple bridges. The higher the case complexity, the more critical it becomes to evaluate a lab’s precision standards, digital workflow, and ability to manage risk. For clinicians and procurement managers, recognizing how complexity changes lab requirements is the first step toward avoiding costly remakes and unpredictable timelines.
complex-implant-case-lab-requirements
What defines a “complex” implant case from a production standpoint?
From a manufacturing perspective, a case is considered complex when it involves multiple implants, long-span frameworks, or advanced biomechanical demands. Full-arch restorations, All-on-4 cases, and hybrid bridges all introduce unique design challenges, where minor inaccuracies in scanning, margin definition, or screw channel angulation can lead to misfits. This complexity pushes the lab to use advanced design tools, precise milling protocols, and experienced technicians capable of anticipating common complications.
How different case types (full arch, All-on-4, hybrid bridges) affect lab requirements
| Case Type | Production Challenges | Lab Requirements |
|---|---|---|
| Full Arch | Large-span frameworks, uniform occlusion | Advanced CAD/CAM, zirconia or titanium milling, precise occlusion mapping |
| All-on-4 | Angulated screw channels, immediate load | Digital planning software, guided surgery compatibility, custom abutment fabrication |
| Hybrid Bridge | Mixed-material workflow, esthetics + strength | Multi-material integration (metal + ceramic), skilled layering technicians, strong QA checkpoints |
These case types represent the most demanding workflows in implant prosthetics. For example, reviewing the Straumann EXACT™ fully digital full‑arch workflow provides clarity on the process rigor a lab must demonstrate and helps procurement teams assess whether a provider can consistently meet high-complexity demands.
Why complexity demands higher precision, planning, and communication
- Higher precision: Complex frameworks allow little tolerance; labs must consistently deliver micron-level accuracy.
- More detailed planning: Digital previews, surgical guides, and staged approvals are essential to avoid late-stage errors.
- Stronger communication: Frequent feedback loops between clinic and lab help prevent mismatches in fit, esthetics, or occlusion.
When these three factors align, complex cases become predictable and repeatable. If any is missing, risks of remakes, delays, or compromised outcomes increase significantly.
Selecting a lab for complex implant cases means looking beyond price or basic turnaround time. It requires evaluating how well the lab adapts its technology, processes, and communication to handle high‑stakes restorations—a differentiation often seen in a specialized overseas dental lab partner.
How Proven Experience with Complex Cases Builds Lab Credibility
A dental lab’s credibility in complex implant cases is not built on claims but on evidence. Procurement managers and clinicians look for verifiable case histories—such as documented success with full-arch restorations, screw-retained frameworks, or multi-unit designs—to confirm that a lab has already solved similar challenges. Trial cases, digital previews, and case records are the clearest ways to separate proven expertise from untested promises.

dental-lab-experience-validation
What types of implant cases indicate lab complexity readiness?
- Full-arch frameworks: Demonstrate ability to manage long-span occlusion and passive fit.
- All-on-4 and All-on-6: Require proficiency with angulated screw channels and immediate loading.
- Hybrid bridges: Show if the lab can integrate metal and ceramic consistently.
- Multi-unit screw-retained cases: Reveal whether the lab maintains accuracy across multiple implants.
These case types function as industry benchmarks. A lab that repeatedly delivers them successfully is more likely to handle the uncertainties of high-stakes restorations.
Why to ask for trial cases, virtual previews, or before-after documentation
Requesting a trial case or digital preview gives clinics tangible evidence of how the lab works. For example, producing a virtual model in 3Shape or exocad allows both sides to confirm margins, screw channels, and esthetic expectations before production begins. Documented before-and-after records provide an additional safeguard that planned outcomes match delivered restorations. A useful reference is a peer-reviewed study on digital full-arch workflows, which highlights why documentation is central to clinical predictability.
How to verify full arch, screw-retained, and multi-unit case proficiency
- Request anonymized CAD designs from prior multi-unit or full-arch projects.
- Check material diversity to ensure success across zirconia, titanium, and hybrid frameworks.
- Review consistency metrics, such as documented remake rates on complex orders.
- Run a pilot order, using one or two trial cases to confirm quality before scaling up.
This step-by-step process ensures procurement teams evaluate performance in real production contexts, not just marketing slides.
Labs that openly share documented case results and allow trial verification build stronger trust than those offering generic assurances. As an overseas dental lab, showing evidence of repeated success with complex restorations signals both technical competence and a collaborative mindset—qualities that give clinics confidence to expand cooperation.
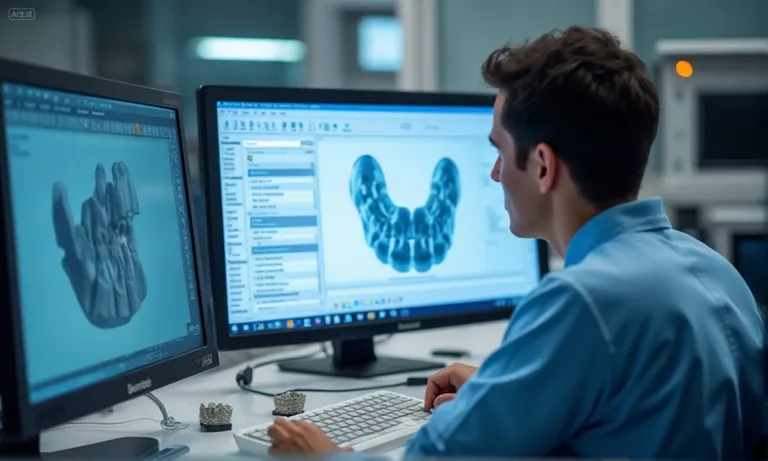
Key Technical Capabilities for Complex Implant Cases
The ability of a dental lab to handle complex implant restorations depends largely on its technical infrastructure. Advanced planning platforms, custom abutment design, and cross-system compatibility form the foundation that allows high-precision, repeatable outcomes. Without these capabilities, even experienced technicians face higher remake rates and inconsistent results.
dental-lab-technical-capabilities-exocad
How virtual planning platforms (e.g., 3Shape, exocad) help manage complexity
Digital planning tools such as 3Shape Implant Studio or exocad DentalCAD allow precise mapping of implant positions, angulation, and occlusal forces before production. This step reduces human error and supports guided surgery protocols. Studies confirm that CAD/CAM-based planning significantly improves implant fit accuracy compared with conventional workflows (PubMed study on CAD/CAM accuracy).
Why custom abutments and multi-unit frameworks require system precision
- Custom abutments: Essential for managing angulated screw channels, ensuring proper emergence profiles, and achieving esthetic integration.
- Multi-unit frameworks: Require tight tolerance in milling so that passive fit is maintained across several implants.
- System precision: Compatibility with leading implant systems prevents misalignment, even when restorative parts come from different suppliers.
Together, these capabilities determine whether a lab can handle All-on-4 or hybrid bridge cases without multiple remakes.
How software and scanner compatibility affect restoration accuracy
| Factor | Risk if Absent | Capability in a Qualified Lab |
|---|---|---|
| CAD software (3Shape, exocad) | Design mismatch or unsupported workflows | Seamless file exchange with clinical scanners |
| Intraoral scanner input | Data loss, margin errors | Accepts multiple formats (STL, PLY, DCM) without distortion |
| Cross-platform integration | Workflow interruptions | Ability to integrate guided surgery, milling, and design approvals |
This compatibility ensures that regardless of which scanner or system a clinic uses, the lab can accept, process, and return accurate restorations.
Technical readiness is not a single tool but an ecosystem: planning platforms, precision milling, and system compatibility must work together. A specialized overseas dental lab that invests in these capabilities helps clients reduce remake risks and gain confidence in delivering predictable, high-value outcomes for complex implant cases.
Which Materials Work Best for Complex Restorations?
The choice of material directly determines whether a complex implant restoration can achieve long-term stability. Unlike single crowns, large-span or hybrid frameworks carry higher mechanical loads and require superior biocompatibility. Zirconia, titanium, and hybrid combinations remain the most trusted options in demanding cases, and evaluating how a lab handles these materials is a key step in supplier selection.

Image
ALT: dental-implant-materials-zirconia-titanium-hybrid
Prompt: A highly realistic, ultra-detailed, professional-quality photo captured in a clean, well-lit environment. Materials must be photorealistic, and rendered with DSLR-level clarity. Lighting should be soft daylight or studio white light. A set of labeled dental implant frameworks (zirconia, titanium, hybrid) displayed on a clean workbench with soft shadows in a professional overseas dental lab environment.
What materials are suitable for long-span restorations (zirconia, titanium, hybrid)?
- Zirconia: High strength, esthetics, excellent for full-arch frameworks; requires precise milling to prevent fractures.
- Titanium: Proven long-term durability, excellent load resistance, biocompatibility for patients with high bite force.
- Hybrid designs (metal + ceramic or PMMA): Balance strength and esthetics, especially for provisional or esthetic-driven cases.
How to assess biocompatibility and mechanical reliability for complex designs
Biocompatibility is a primary concern in full-arch or multi-unit cases because restorations interact with both soft tissue and bone. Materials must avoid inflammatory reactions and withstand years of function. Clinical evidence shows that zirconia and titanium both achieve predictable integration, though titanium offers higher load-bearing reliability (comparative study on zirconia vs. titanium frameworks). Hybrid solutions, while versatile, should be carefully assessed for wear over time, particularly in patients with parafunctional habits.
Whether the lab can manage mixed-material workflows (e.g. metal + ceramic)
| Workflow Type | Typical Use | Key Lab Requirements |
|---|---|---|
| Metal + ceramic layering | Final esthetic restorations | Skilled technicians, precise firing protocols |
| Titanium + acrylic (PMMA) | Long-term provisional or immediate load | Digital planning, strong bonding interface |
| Zirconia with gingival ceramic | Full-arch with esthetic demand | Layering consistency, shade matching |
Labs capable of handling these combinations can offer both functional reliability and esthetic refinement. The ability to switch or combine materials also reflects maturity in workflow integration.
Material selection in complex implant restorations is not only a technical choice but a strategic safeguard. A specialized overseas dental lab with proven multi-material expertise helps clients balance esthetics, function, and longevity, making long-span and hybrid cases more predictable and sustainable.
For large-span restorations, mechanical reliability is equally critical: titanium withstands high bite forces, while zirconia requires careful thickness planning to avoid structural failure. Hybrid solutions extend flexibility but should be carefully evaluated for long-term wear.
Whether the lab can manage mixed-material workflows (e.g. metal + ceramic)
| Workflow Type | Clinical Use | Lab Requirement |
|---|---|---|
| Metal + ceramic layering | Esthetic anterior cases | Skilled technicians, precise firing cycles |
| Titanium + acrylic (PMMA) | Long-term provisional or immediate-load | Digital bonding protocols, CAD/CAM verification |
| Zirconia + ceramic gingiva | Full-arch with high esthetic demand | Consistent layering and shade matching |
A lab with the ability to process multi-material workflows ensures both functional stability and esthetic harmony. This versatility is especially important in full-arch and hybrid cases where patient demands vary widely.
In summary, material selection in complex implant restorations is not only about esthetics but about mechanical resilience and biological safety. Partnering with an overseas dental lab that has proven expertise across zirconia, titanium, and hybrid systems gives clinicians confidence in long-term outcomes.
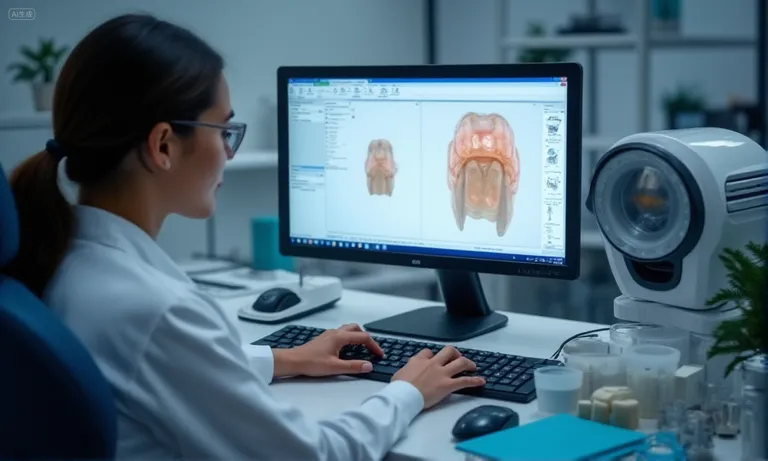
How Strong Lab Communication Reduces Design and Fit Risks
Clear and consistent communication between clinicians and labs is one of the most effective ways to reduce design errors and misfit risks in complex implant cases. Multi-unit frameworks and full-arch restorations demand careful coordination, because even small misunderstandings can cause costly remakes. Strong protocols, digital previews, and structured feedback loops create safeguards that improve predictability and reduce chairside adjustments.

Image
ALT: dental-lab-digital-feedback-loop-implant-case
Prompt: A highly realistic professional photo showing a dentist and dental technician collaborating online. The computer screen displays a 3D digital implant framework with annotations. The scene is captured in a modern overseas dental lab environment with clear lighting and professional focus.
What protocols should labs follow for case design verification?
- Detailed prescriptions – Digital prescriptions should clearly define implant position, angulation, and restoration type.
- Standardized checklists – Verification at scanning, CAD design, and milling ensures fewer missed details.
- Approval checkpoints – Clinician confirmation before milling prevents irreversible design errors.
Why feedback loops and digital previews help refine implant outcomes
Digital platforms such as exocad or 3Shape allow clinicians to preview frameworks before fabrication. This step supports real-time design refinements and minimizes downstream risks. Research highlights that collaborative review of digital workflows improves restoration accuracy and reduces remake rates (NCBI article on digital workflows in implant dentistry). For full-arch and multi-unit cases, this is particularly critical, as a misfit may require extensive chairside adjustments or even a full remake.
How to ensure technician-clinician alignment throughout the process
- Case submission clarity – Ensure scans and prescriptions are complete.
- Shared digital workspace – Both parties view and annotate the same 3D file.
- Scheduled review checkpoints – Align expectations before and after milling tests.
- Final verification meeting – Confirm occlusion, fit, and esthetics before delivery.
Effective alignment is not just administrative—it is a technical control point. As an overseas dental lab, we integrate structured communication and feedback loops into every complex case, helping clinicians reduce risks and improve patient outcomes.
What QA Processes Ensure Stability for Full Arch and Hybrid Cases
High-complexity implant restorations, such as full-arch or hybrid cases, require stricter quality assurance (QA) because remake rates are significantly higher compared to single-unit crowns. Each production stage—scanning, CAD design, milling, and finishing—must follow structured QA protocols to ensure consistent fit, function, and durability.

dental-lab-quality-assurance-checkpoints
Why remake rates tend to rise with complexity—and how good labs manage it
The more implants and units involved, the higher the cumulative tolerance stack-up, leading to greater risks of misfit. According to the National Institutes of Health, complex prostheses show higher variability in fit due to multiple manufacturing steps (NIH study on implant-supported prostheses). A strong QA system reduces this variability by detecting errors early, preventing costly remakes and protecting clinical schedules.
What QA checkpoints matter in scanning, milling, and finishing
- Digital scan verification – Checking for distortions, missing areas, and proper occlusal capture.
- CAD design validation – Reviewing emergence profiles, screw access positioning, and multi-unit connection accuracy.
- Milling tolerance control – Ensuring machines are calibrated and materials are processed within manufacturer guidelines.
- Finishing inspection – Technician review under magnification to confirm marginal integrity and surface smoothness.
- Final trial fitting (virtual or physical) – Verifying seating accuracy before delivery.
How to evaluate lab consistency for implant-supported multi-unit cases
| Evaluation Area | What to Look For | Lab Indicator |
|---|---|---|
| Remake rates | Should be <5% for complex cases | Historical performance data |
| QA documentation | Stage-by-stage verification records | Transparent reports shared with clients |
| Case reproducibility | Similar outcomes across different technicians | Internal peer-review of completed cases |
| Material testing | Regular checks for zirconia strength, titanium surface quality | Lab provides certificates of conformity |
| Calibration control | Machines regularly maintained and validated | Documented maintenance logs |
By embedding these QA measures into the workflow, an overseas dental lab can provide clinicians with confidence that even demanding full-arch or hybrid cases will be delivered consistently and predictably. Peer-reviewed studies confirm that adherence to standardized QA protocols reduces variability and increases clinical success rates (Wiley study on quality management in dental manufacturing).
In summary, QA in complex implant restorations is not just about defect prevention—it is about building a reproducible system. A well-structured lab ensures stability by reducing remake risk, maintaining consistent results, and giving clinicians reliable outcomes for their most challenging cases.
How Complexity Impacts Turnaround Time and Delivery Expectations
Turnaround time for complex implant cases is longer than for standard crowns. Full-arch, All-on-4, and hybrid restorations involve more design, milling, and QA stages, adding several working days to production cycles. Clinics that plan with realistic timelines prevent patient scheduling disruptions and reduce stress.

dental-lab-turnaround-time-all-on-4
What is a realistic lead time for high-complexity cases like All-on-4?
While a single-unit crown may be delivered in 3–5 days, full-arch zirconia restorations typically require 10–15 working days, and hybrid cases can extend further. The FDA acknowledges that multi-step workflows in dental device manufacturing demand extra validation time (FDA guidance on dental device manufacturing). Aligning delivery expectations prevents clinical delays and supports smoother scheduling.
How complexity affects scheduling, logistics, and rush-case feasibility
- Each stage—design, milling, finishing—needs its own validation and cannot be rushed without raising risks.
- International shipping and customs add 2–4 days, especially for expedited cases.
- Rush orders often compromise QA protocols and are generally discouraged unless absolutely necessary.
- Building in a 2–3-day buffer provides essential coverage against unforeseen delays.
What to clarify about lab capacity and multi-case coordination
Even with advanced equipment, a lab’s human capacity—technician availability and scheduling systems—dictates consistency. Published studies emphasize that reliable scheduling systems improve on-time delivery in dental labs. As an overseas dental lab, we advise coordinating volume expectations upfront to ensuring smooth delivery across multiple complex restorations.
In summary, complexity extends production cycles—but with transparent planning and communicated capacity, reliable timelines are achievable. Labs that proactively share expected lead times, processing buffers, and QA checkpoints partner better with clinics and support uninterrupted patient care.
Conclusion
Choosing the right lab partner for complex implant restorations requires more than cost evaluation—it demands proven experience, strong digital capabilities, robust QA systems, and transparent communication. From full-arch zirconia frameworks to hybrid bridges, every stage of production introduces variables that must be carefully managed to ensure predictable outcomes. By partnering with an overseas dental lab that combines advanced digital workflows, material expertise, and consistent scheduling, clinicians can reduce remake risks and improve long-term treatment reliability. Clear alignment between the clinic and lab ultimately transforms complexity into a predictable, collaborative process.