As crown and bridge manufacturing evolves, dental labs are adopting technologies that promise greater precision, faster turnaround, and improved consistency. But for procurement professionals, the key question is no longer who has the latest tools—it’s who uses them effectively to deliver measurable outcomes.
From 3D printing and AI-assisted design to advanced milling workflows and high-performance materials, each innovation introduces both opportunity and complexity. Some labs implement these technologies with proven results—others simply add them to a capabilities list.
This article breaks down seven evaluation areas to help procurement teams assess a lab’s true digital readiness:
- Assess how new technologies affect lead times, accuracy, and clinical consistency
- Compare use cases of 3D printing vs. traditional milling in restorative workflows
- Understand how AI and automation impact design reliability and technician workload
- Review advancements in CAM systems and 5-axis milling for bridge cases
- Evaluate the clinical value of multilayer zirconia and hybrid ceramics
- Determine if lab staff, protocols, and QA systems are ready for scaled implementation
- Use structured vetting questions to uncover real-world maturity and alignment
These insights equip buyers to move beyond marketing claims—toward partnerships with labs that are not only tech-capable, but also workflow-aligned, reliable, and ready to scale with modern dental demands.
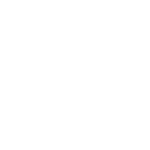
Why Are New Technologies Transforming Crown and Bridge Manufacturing?
New technologies are reshaping crown and bridge manufacturing by driving improvements in precision, efficiency, and scalability—all essential for meeting modern clinical and procurement demands. Labs that embrace advanced digital systems are better positioned to deliver faster turnarounds, tighter quality control, and predictable outcomes across complex restorative cases.

dental-lab-digital-transformation-equipment-overview
What factors are driving innovation in crown and bridge production?
Innovation in crown and bridge production is driven by evolving clinical expectations and the pressure for higher efficiency in dental workflows. Key drivers include:
- Increased demand for esthetic outcomes: Patients expect lifelike restorations, pushing labs to adopt materials and technologies that mimic natural teeth.
- Multi-unit complexity: Full-arch and implant-supported bridges require more design accuracy, leading to adoption of digital simulation and validation tools.
- Cross-border scalability: Labs serving DSOs or international clinics need standardized systems that support volume and consistency across geographies.
- Chairside integration: Clinicians now expect digital labs to align with intraoral scanning and design software for streamlined case transfers.
- Competitive pressure on lead times: Buyers are increasingly favoring labs with faster, traceable turnaround systems driven by automation and digital coordination.
At Raytops, we saw case volumes triple for multi-unit zirconia in the past 18 months—driven in part by DSOs shifting to fully digital design protocols. This growth would not have been manageable without scalable digital tooling and pre-milling validation steps.
How do new technologies impact quality, consistency, and lead times?
The adoption of digital technologies significantly enhances multiple performance metrics.
| Impact Area | Traditional Workflow | Tech-Enabled Workflow |
|---|---|---|
| Quality control | Manual checks, visual only | Digital margin validation, connector analysis |
| Consistency | Technician-dependent output | Template-driven, repeatable CAD designs |
| Lead time | 7–10+ days avg. (manual steps, shipping) | 3–5 days avg. with digital-first case intake |
Clinics working with digital-first labs consistently report smoother seating experiences, fewer remakes, and better predictability in patient scheduling—especially in cases involving 4+ units or esthetic zones.
Why should buyers track these technology developments?
Because the quality of your restorative outcomes—and your procurement efficiency—now depends on how tech-enabled your lab partner is. Buyers who don’t assess this risk working with labs that may fall behind in accuracy, speed, or traceability.
In 2023, a U.S.-based procurement lead told us their previous lab couldn’t align scanned data from their Trios systems with final zirconia designs—resulting in four remakes across two months. After switching to a lab with native scanner integration, remake frequency dropped by over 70%.
Whether you’re sourcing for a DSO, private clinic, or distributor, understanding a lab’s digital maturity isn’t optional anymore—it’s operationally essential.
What Role Does 3D Printing Play in Crown and Bridge Workflows?
3D printing is becoming a critical enabler in crown and bridge workflows—offering speed, precision, and flexibility in areas where milling or manual work may fall short. For buyers and procurement teams, the key is not just whether a lab owns a printer, but how well that technology is integrated into the restorative process with validated materials and protocols.

dental-lab-3d-printing-model-prosthetic-comparison
What are the main 3D printing applications in dental prosthetics?
In crown and bridge workflows, 3D printing is primarily used to accelerate support processes—not always final restorations. Key applications include:
- Printed working models: Created from intraoral scans for try-ins, final verification, or technician referencing.
- Surgical guides and temporaries: Printed in biocompatible resin for implant positioning or provisional use.
- Try-in prototypes: Useful for esthetic and functional checks before final milling or pressing.
- Custom trays and bite splints: Printed on demand, reducing lab setup time.
In our lab, we routinely print resin models for complex anterior cases where shade and contour need technician validation before final pressing. It allows for same-day feedback loops with clients using digital viewers.
How do printed prosthetics and models compare to milled versions?
While 3D printing offers flexibility and cost savings, its performance varies depending on application and post-processing quality.
| Application Type | Milled Version | 3D Printed Version |
|---|---|---|
| Working models | Highly durable, slow to produce | Faster, lower cost, less abrasion-proof |
| Provisional crowns | Limited esthetics | High esthetics, suitable for short term |
| Full-contour crowns | Superior strength | Not yet widely validated for final use |
| Custom trays/bite guards | CNC-formed, durable | Cost-effective, easier to iterate |
Printed models are ideal for diagnostics and temporaries, but final crowns still favor milling or pressing due to strength and long-term intraoral stability.
How should buyers evaluate print precision, validation, and materials?
Procurement teams should look beyond brand names and ask for evidence of print calibration, resin certification, and case-level validation. Good questions include:
- Are printed models regularly benchmarked against milled ones for dimensional accuracy?
- Is the resin FDA-cleared or CE-marked for its intended use (e.g., try-in vs. provisional)?
- How often is printer calibration verified—and is a log available?
- Are post-processing protocols (e.g., UV curing, cleaning) standardized?
A distributor client in Australia once reported bite misalignment across printed models from a previous lab. Upon review, we discovered they were skipping post-cure exposure times. After standardizing their curing cycles and introducing batch control logs, remake rates dropped by 60% over the next 6 weeks.
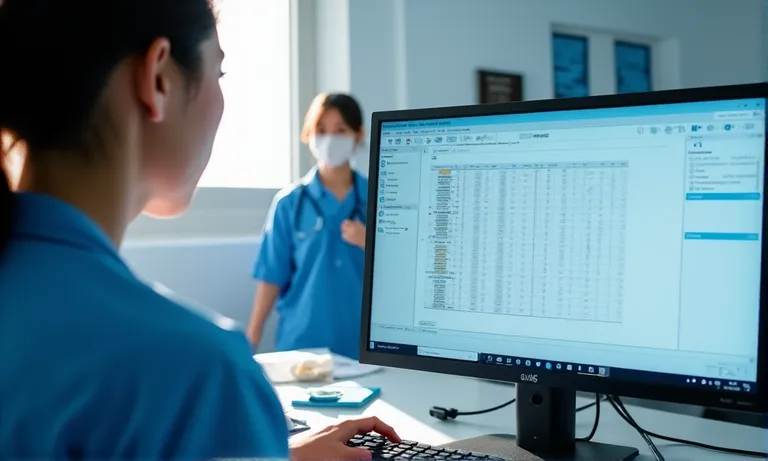
How Are AI and Automation Enhancing Dental Lab Operations?
AI and automation are streamlining core steps in dental lab workflows—from margin detection to model segmentation—while reducing manual variability and increasing throughput. But alongside the benefits come real considerations: how much control is retained, what gets validated, and where over-reliance may lead to risk.

dental-ai-margin-detection-vs-manual-design
How is AI used in design segmentation and margin detection?
AI has become particularly effective in early-stage design tasks where speed and repeatability matter most.
- Margin line detection: AI-assisted systems like 3Shape’s Margin Wizard now detect finish lines within seconds, improving turnaround and reducing technician fatigue.
- Tooth segmentation: Automated tooth region mapping streamlines the design of multi-unit bridges and helps reduce anatomical errors.
- Connector suggestions: Some systems suggest connector width and position based on span and case type.
- Automated checks: Algorithms can flag undercuts, irregular emergence profiles, or insufficient occlusal clearance.
In our workflow, AI tools are often used to generate the first design pass. Technicians then refine and validate output—ensuring both speed and clinical relevance remain balanced.
Can automation improve design accuracy and reduce human error?
When used properly, automation can standardize high-variability steps and eliminate fatigue-driven errors.
| Workflow Step | Manual Execution | AI/Automation Support |
|---|---|---|
| Margin marking | Technician-dependent, variable across shifts | Consistent output with visual confidence score |
| Bridge connector sizing | Manual input prone to miscalculation | AI suggests optimal width based on span |
| Occlusion adjustment | Relies on technician feel | Simulated occlusal analysis pre-manufacturing |
We’ve worked with several labs scaling up full-arch workflows who found that switching to AI-based connector validation reduced fracture-related remakes by 40% in under 3 months.
What risks come with over-relying on automation?
Over-automation without technician oversight can introduce blind spots—particularly in complex, esthetic, or borderline-prep cases.
A DSO client once submitted a 4-unit anterior case for automated margin detection. The system misinterpreted a subgingival margin on lateral #7, producing a short crown. The lab had skipped visual verification due to high volume. The case was remade—delaying the patient appointment and increasing tension with the clinic.
Procurement teams should ask labs not just if they use AI, but how oversight is maintained. Responsible automation means human-in-the-loop protocols, approval checkpoints, and risk-based exceptions—not blind handoffs.
What’s New in Milling Equipment and CAM Workflow?
Recent advancements in milling and CAM technologies have redefined how dental labs handle anatomical complexity, speed, and restoration predictability—especially in full-arch and multi-unit bridge cases. For procurement teams, understanding what equipment a lab uses (and how they use it) directly affects case consistency, margin integrity, and structural longevity.

5-axis-dental-milling-cam-zirconia-bridge-workflow
How does 5-axis milling improve bridge anatomy accuracy?
Five-axis milling allows for angulated drilling paths and smoother undercut access, significantly improving fit and anatomical precision in curved or multi-unit structures. Compared to 3-axis systems, key improvements include:
- Access to complex angles: Enables milling of undercuts without rotating the model manually.
- Improved connector integrity: Milling from multiple angles ensures even thickness across span lengths.
- Esthetic contouring: Facial anatomy and gingival emergence profiles can be milled with better control.
In our lab, upgrading to 5-axis systems reduced internal adjustment rates on posterior bridges by over 50%—particularly in longer spans where flat-axis systems struggled to maintain connector symmetry.
What are the advancements in zirconia sintering protocols?
New sintering ovens and software allow labs to fine-tune temperature ramps, hold times, and shrinkage compensation—directly improving zirconia strength and shade stability.
| Sintering Parameter | Traditional Oven | Advanced Protocol Capable System |
|---|---|---|
| Ramp-up speed | Fixed default | Adjustable by material and case size |
| Shrinkage compensation | Manual or template-based | Auto-calculated via scanned pre-milled model |
| Shade consistency | May vary by thickness | Profiled by location in furnace and material |
One U.S.-based partner lab we support reported a 35% drop in crown surface cracks after shifting from manual sintering to CAM-integrated furnace scheduling. They also noticed more predictable A1-to-A3 shade results across anterior units.
Are new CAM systems capable of handling highly complex designs?
Yes—but only when paired with trained technicians and consistent input quality. CAM systems now offer:
- Real-time simulation: Allowing for dry-run verification of toolpaths and connector stability before milling.
- Material-specific workflows: Adjusting parameters for lithium disilicate, zirconia, or hybrid materials automatically.
- Error flagging: Highlighting potential tool collisions, thin walls, or unsupported pontics.
However, during a cross-border project with a mid-sized European lab, we found that despite having upgraded CAM software, their technicians used outdated workflows. After joint training and standardization, remake volume fell by 12% over the following quarter.
How Are Advanced Materials Redefining Crown and Bridge Options?
Advanced materials like multilayer zirconia and hybrid ceramics are expanding the possibilities of crown and bridge restorations—offering better shade blending, improved strength-to-thickness ratios, and broader clinical indications. For buyers, knowing what materials a lab offers (and how they’re validated) is key to managing esthetics, function, and longevity.

multilayer-zirconia-hybrid-ceramic-comparison
What’s different about multilayer zirconia and hybrid ceramic materials?
These new materials are engineered to solve longstanding esthetic and structural trade-offs.
- Multilayer zirconia: Designed with gradient shade and translucency zones, allowing for more natural color transitions without manual layering. This reduces post-milling staining and labor time.
- Hybrid ceramics (e.g., Vita Enamic): Combine ceramic hardness with resin elasticity, making them ideal for minimally invasive preps and stress-bearing areas in anterior restorations.
- High-translucency zirconia: Used increasingly in anterior cases where esthetics are prioritized, while still maintaining acceptable flexural strength (>700 MPa in many brands).
In our workflows, we often propose multilayer zirconia for anterior bridge cases where shade transition and cervical blending are critical—cutting down remakes due to shade mismatch by up to 12%.
How do these materials affect shade matching, translucency, and durability?
New-generation materials are more consistent across indications—but each has trade-offs.
| Property | Multilayer Zirconia | Hybrid Ceramics |
|---|---|---|
| Shade Matching | Good intrinsic gradient | Requires surface staining |
| Translucency | Controlled by disc layer | Naturally high, especially in thin areas |
| Flexural Strength | 700–1200 MPa depending on zone | 150–200 MPa |
| Indicated For | Full crowns, bridges, anterior restorations | Inlays, onlays, thin veneers |
| Milling Adjustability | Good for complex frameworks | Easier edge trimming, faster mill time |
We once assisted a UK-based clinic evaluating hybrid ceramics for posterior bridges. The material passed initial esthetic tests but failed under load due to insufficient thickness tolerance. We recommended switching to multilayer zirconia with optimized sintering—a change that led to sustained performance over 14 months of follow-up.
Are there certifications or testing protocols buyers should request?
Yes—labs should be able to provide both material certifications and internal validation data.
- ISO 6872: Confirms the ceramic material meets strength and safety standards for dental use.
- Batch traceability: Ensures any issues can be tracked to a specific material lot.
- Internal test protocols: Many labs now run in-house fatigue or stain resistance tests, especially when evaluating new suppliers.
- Case library or validation report: Some offer anonymized case examples with outcomes, helping buyers judge real-world performance.
When partnering with labs for crown and bridge work, buyers should ask not only what materials are used—but also how those materials are selected, tested, and matched to the clinical context.
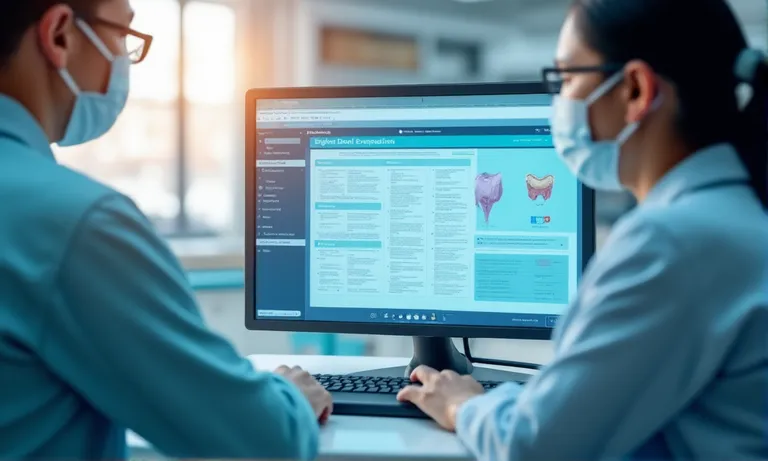
How Can Buyers Evaluate a Lab’s Readiness to Implement New Technologies?
Technology alone doesn’t ensure better outcomes—labs must also demonstrate how well they’ve operationalized it. For procurement teams, evaluating a lab’s tech readiness means looking beyond equipment inventory to assess training depth, workflow integration, and real-world results.
dental-lab-tech-training-dashboard-validation
Do they provide case studies, testing data, or demo workflows?
Labs that are truly tech-enabled should be able to show—not just tell.
- Demo workflows: Step-by-step visuals of how new systems are used in real cases.
- Validation datasets: Shrinkage rates, marginal fit benchmarks, or stress test data on new materials.
- Anonymized case studies: Proof of performance in anterior esthetics, full-arch fits, or time savings after software adoption.
- Before/after comparisons: Showing impact of automation, AI-based segmentation, or new sintering curves.
At Raytops, we often prepare demo sequences for new clients—especially DSOs transitioning to digital workflows. For one Canadian DSO, we provided before/after remake logs and digital screenshots, which directly led to a six-month pilot agreement.
Are staff trained and certified in operating new equipment?
Advanced equipment needs advanced hands.
| Staff Competency Area | Evaluation Questions Buyers Can Ask | Why It Matters |
|---|---|---|
| CAM/Milling Proficiency | Are CAM designers certified or internally benchmarked? | Impacts toolpath precision, connector strength |
| Material Handling | Is staff trained on sintering ovens by manufacturer protocols? | Ensures consistency in final translucency and fit |
| Automation Workflow Use | Can they show staff usage logs or simulation audits? | Reveals real vs. nominal adoption of automation tools |
We once supported an Australia-based clinic evaluating a “fully digital” lab. The lab listed Exocad and 5-axis equipment—but had zero certified users. With no standardized output checks, anterior remake rate was over 30%. Our joint retraining program cut that to 8% in 3 months.
How do they manage the transition between traditional and emerging methods?
Labs still handling mixed analog-digital cases must have clear protocols for crossover and integration.
- Dual-path workflows: Can they combine intraoral scans with analog impressions when needed?
- Digital-to-manual checkpoints: Are there steps where technicians inspect CAD outputs before fabrication?
- Legacy system mapping: Do they have compatibility charts for older software/scanners?
- Transition SOPs: Clear playbooks for migrating recurring cases from manual to digital flow.
Many labs claim digital readiness—but only some offer repeatable, auditable, and scalable systems for applying it. As a buyer, request evidence of maturity—not just availability.
What Questions Should Procurement Teams Ask When Vetting Tech-Enabled Labs?
Great questions uncover weak workflows. For procurement teams, vetting a lab’s digital capabilities requires more than ticking off equipment lists—it calls for asking the right questions to verify operational maturity, track record, and impact on business outcomes.
dental-procurement-vetting-checklist-kpi-dashboard
What is the lab’s proven experience with recent technology adoption?
Experience with tech means little unless it’s operationalized. Key questions include:
- Can you share 2–3 client cases that improved due to this technology?
- What KPIs changed after adopting [e.g., AI segmentation or 5-axis milling]?
- How long did it take to integrate the new system into your daily workflow?
Labs that answer these with data-backed specifics—not vague anecdotes—are more likely to deliver stable performance. In one case, a US DSO uncovered during vetting that a lab advertising “AI-enhanced design” hadn’t rolled it out beyond demo files. That lab was eliminated before trials, avoiding downstream delays.
Can they demonstrate how specific technologies improve buyer outcomes?
Procurement is impact-driven. Structure your vetting around outcome questions:
| Evaluation Angle | Suggested Question | Why It Matters |
|---|---|---|
| Turnaround Impact | Has automation reduced turnaround variance in complex cases? | Affects scheduling and patient coordination |
| Esthetic Consistency | Do you have data on shade remakes pre- and post-new materials? | Critical for anterior work and patient satisfaction |
| Case Transparency | Can we track digital checkpoints across workflow stages? | Impacts QA visibility and remote approvals |
At Raytops, when onboarding group practices, we prepare “impact briefing slides” linking technology use (e.g., new sintering curves) with before/after remake rates. One client reported a 19% drop in remake requests within 90 days of switching labs based on these insights.
Are there clear cost implications, timelines, or onboarding support?
Uncertainty kills deals. End your vetting with logistical clarity:
- What is the total onboarding timeline, from first test file to regular orders?
- Are there any price differences for digitally processed vs. traditional cases?
- What support is provided during the trial phase—tech setup, staff orientation, or material coordination?
Labs that clearly map cost structures and onboarding expectations build trust early and reduce the risk of surprise escalations post-contract.
Conclusion
Adopting new technologies is no longer optional—it’s a strategic imperative for labs supporting crown and bridge cases at scale. For procurement teams, evaluating a partner’s digital maturity means asking the right questions, assessing real-world implementation, and verifying outcome-based improvements.
Labs that successfully integrate AI, 3D printing, advanced milling, and next-gen materials can offer better consistency, faster turnaround, and more predictable collaboration. But true readiness lies not in tool ownership, but in how these tools are used to support daily workflows.
As an overseas dental lab deeply involved in digital transitions, we’ve seen how the right infrastructure—combined with process discipline—can directly improve client satisfaction and remake rates. The right technology partner isn’t just advanced—they’re aligned.