Choosing the right dental lab for 3D printing involves more than reviewing technical specs—it requires asking the questions that reveal real-world reliability. For dental clinics, DSOs, and lab-to-lab partners, evaluating a lab’s accuracy, materials, and workflow readiness is essential to ensuring long-term success.
This practical framework helps procurement and operations teams assess whether a lab is prepared to deliver consistent, scalable 3D printed restorations by focusing on six key areas:
- Accuracy assurance: measurement protocols, quality control processes, and defined tolerances
- Material compatibility: certified resins, biocompatibility standards, and indication-specific choices
- Workflow integration: file format acceptance, scan handling, and data error resolution
- Performance benchmarks: turnaround times, remake rates, and production consistency
- Validation evidence: real case samples, ISO certifications, and referenceable client outcomes
- Support structure: equipment transparency, troubleshooting workflows, and responsiveness
By using these criteria, decision-makers can confidently identify which labs are not only 3D printing–capable—but also digitally aligned, operationally reliable, and ready to support clinical demands at scale.
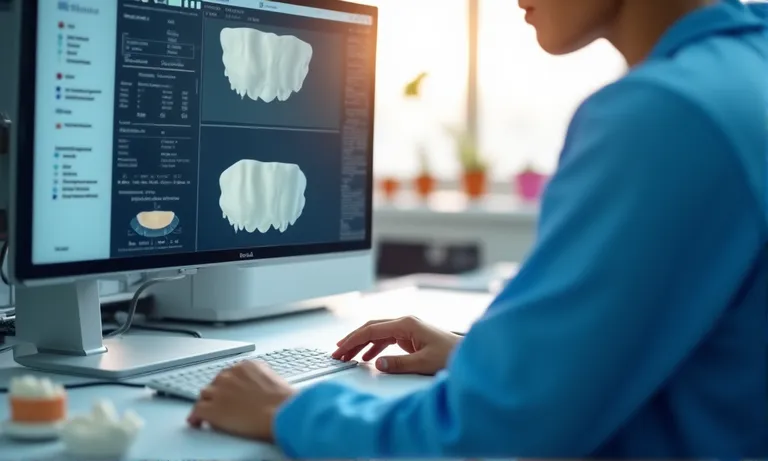
What Questions Reveal a Lab’s 3D Printing Accuracy Standards?
A qualified dental lab should clearly explain how they measure, monitor, and act upon 3D printing accuracy metrics—such as marginal gap tolerances and quality control checkpoints—to ensure consistent fit and reduce remakes. Don’t settle for vague claims—ask for numbers, processes, and error-handling methods.
3D printing accuracy isn’t just about machines—it’s about measurable standards, consistent validation, and transparent correction mechanisms. Here’s how to dig deeper into a lab’s true capability.

dental-lab-printing-accuracy-check
How does the lab measure printing accuracy for crown and bridge components?
Labs that take accuracy seriously can demonstrate how they assess it. Precision often focuses on marginal gap (typically measured in microns) and internal fit between printed models and final restorations.
Key indicators to ask about:
- Verification methods: Does the lab use digital calipers, 3D comparison software, or microscope inspection?
- Measurement frequency: Are random checks done per batch or per case?
- Calibration protocol: Are their printers and resins calibrated with each material batch?
For example, in our lab, we perform digital deviation mapping using 3Shape’s Compare tool on sample batches weekly. Accuracy metrics are recorded in our internal QA dashboard for trend monitoring.
What tolerance thresholds does the lab use in printed dies or wax-ups?
Understanding a lab’s tolerance range gives you insight into their manufacturing precision. Here’s how typical thresholds compare with quality benchmarks:
| Component Type | Industry-Acceptable Tolerance | High-Accuracy Lab Standard (e.g. Raytops) |
|---|---|---|
| Printed Dies | ±50–70 µm | ±30 µm |
| Wax Patterns (C&B) | ±70–100 µm | ±40 µm |
| Implant Models | ±30–50 µm | ±20 µm |
These small numbers have a big impact on fit, cement space, and adjustment time. Labs that exceed these tolerances consistently risk poor-fitting prosthetics and chairside rework.
How are discrepancies detected and handled during quality control?
Even top labs occasionally produce deviations—what matters is how they detect and respond. A trustworthy lab should walk you through their QA protocol, including how they handle issues like layer shifting, surface artifacts, or material distortion.
A mid-sized Australian clinic flagged a consistent issue with printed dies not seating flush. Our QA review found the root cause—printer drift during longer print runs. We recalibrated the build plate, changed the print batch size, and implemented a new inspection checkpoint for surface flatness. After that, their complaint rate on dies dropped to zero over three months.
The lesson? You don’t just want precision—you want a partner who monitors, responds, and improves over time.
Labs that hold ISO 13485 standard or have well-documented internal QA processes are more likely to catch and correct print errors before they reach your practice. Always ask for evidence of such systems.
By asking the right questions, you can spot whether a lab is engineering quality—or merely promising it.
What to Ask About 3D Printing Materials and Indications?
Key takeaway: The right questions about material selection, certification, and performance can help you identify whether a dental lab’s 3D printing capabilities align with your clinical requirements—not just technically, but in long-term biological safety and reliability.
All 3D printable materials are not created equal. Some are suitable for short-term intraoral use; others lack regulatory clearance. To ensure predictable results and avoid complications, clinicians and lab partners must align on material performance and certification.

dental-lab-3d-printing-material-selection
What printable materials does the lab offer for temporary crowns or frameworks?
Different clinical indications require different materials—especially when the restoration is placed in the mouth. Temporary crowns, surgical guides, custom trays, or long-span frameworks all require biocompatible and dimensionally stable resins.
Here’s what to confirm:
- Material type and brand: Is the resin from a known manufacturer (e.g. NextDent, KeyPrint)?
- Application-specific selection: Does the lab recommend different resins for long-term temps vs. short-term diagnostic use?
- Resin aging and storage protocols: Are they tracking batch numbers and expiration?
Knowing what they print with—and how—is the foundation for trusting the final restoration.
Are the materials certified for dental use (e.g. FDA, CE)?
Certification is not optional—it’s the baseline for safety. Ask the lab to provide documentation for any intraoral-use resin, especially those used for temporaries and surgical guides.
| Certification Type | Relevance in Clinical Context |
|---|---|
| FDA 510(k) or Class II | Required for US-market biocompatibility assurance |
| CE Certification | Valid for EU-based usage; ensures MDR compliance |
| Internal QA Protocol | Reinforces lab’s process rigor even for certified materials |
Without certified materials, there’s no guarantee on tissue safety, allergic response, or intraoral performance.
How does the lab verify dimensional stability or biocompatibility?
Material safety isn’t just about documentation—it’s about real-world performance. One of our clients, a three-chair clinic in southern Spain, noticed that some printed temporaries warped within 48 hours when stored in sunlight-facing containers. After reviewing their handling workflow, we discovered their local lab didn’t post-cure under validated conditions.
When the cases shifted to our workflow, we made sure all long-term temps used a CE-certified resin and were post-cured using manufacturer-defined UV cycles. Since then, their return rate on temps has dropped below 1% across six months.
We also now share post-curing parameters transparently in our delivery report, so clinics can trace not just the resin—but how it was handled.
If your lab can’t explain the relationship between curing, stability, and clinical performance, that’s a red flag. Ask not only what they use, but how they process it.
What Questions Uncover Workflow Compatibility and Data Handling?
A lab’s ability to handle diverse file types, resolve data discrepancies, and integrate into your digital workflow directly affects case accuracy and turnaround speed. Clarifying these processes upfront reduces costly delays later.
Even the best restorations can fail if the upstream digital process is misaligned. That’s why understanding how your lab processes data—from file intake to scan conversion—is critical in evaluating real digital readiness.
dental-lab-digital-workflow-integration
What file formats (e.g. STL, PLY) does the lab accept and process?
A digitally competent lab should handle multiple scan sources and formats without data loss. Ask which input types they support—and whether they optimize those formats before production.
Key compatibility questions:
- Accepted formats: STL, PLY, OBJ—are they all supported?
- Compression handling: Does the lab reprocess compressed scans?
- Metadata preservation: Are color, margin lines, or embedded prep guides retained?
If the lab regularly handles files from TRIOS, iTero, Medit, and others, they should be able to describe how they maintain detail through each step.
How does the lab integrate intraoral scans into the 3D printing workflow?
When intraoral data flows directly into model printing, small differences in file handling or segmentation can snowball into big errors.
Here’s how the process typically works when done right:
- File intake and validation
All incoming scans are checked for completeness and occlusion alignment. - Margin and prep area inspection
Design software highlights undercuts, voids, or blurry zones. - Segmentation for model building
Files are converted for physical printing (often with removable dies or implant analogs). - Print-ready verification
A secondary technician cross-verifies model base geometry and contacts.
Ask your lab if this kind of double-checking is standard—or only done on request.
What happens if file errors or mismatches occur?
Even with good systems, data mismatches can happen. What matters is how quickly and transparently the lab responds.
One of our DSO clients in Canada experienced recurring issues where TRIOS scans sent via cloud would arrive without occlusal alignment tags. Instead of sending the case back, we built an internal protocol to flag such cases, then proactively contacted the clinic for chairside re-scan or alternative occlusal data. Over two months, their file rejection rate dropped from 8% to under 1%.
Since then, we’ve embedded a “file check + confirm” step into our onboarding SOP for any new scanner integration.
Labs that treat file problems as a collaboration opportunity—not just rejection reason—will save you significant clinical time.
What Operational Metrics Should You Ask the Lab to Share?
Labs that openly share data—like turnaround time, remake rate, and batch consistency—signal operational maturity and help you manage expectations, identify risks, and build long-term trust.
It’s not just about how nice the final crown looks—it’s about whether you’ll receive it on time, with minimal rework, and consistent quality from one case to the next.

dental-lab-production-metrics-dashboard
What is the average turnaround time for 3D-printed components?
Time matters—especially for temporary restorations and multi-unit cases. But not all labs define turnaround time the same way.
Key follow-up questions:
- From when to when: Does it count from scan received or design approved?
- Printed part vs. full case: Are you asking about the model print or crown delivery?
- Buffer days: Do they build in courier slack or process rechecks?
Most reliable labs publish clear timelines per product. For example, average turnaround for a printed model is 24–36 hours, while full crown cases may be 4–6 working days. You can compare this to industry benchmarks for context.
What is the remake or adjustment rate for printed crown/bridge cases?
A lab’s remake rate is a window into their upstream quality control. Here’s a common metric table:
| Metric | Industry Average | Raytops Internal Target |
|---|---|---|
| Remake Rate (All Cases) | 4–6% | <2% |
| Chairside Adjustment Frequency | 12–18% | <8% |
| Model Reprint Trigger Rate | ~3% | <1% |
Ask whether their remake numbers include digital-only reprints or just physical redeliveries. Labs with better tracking often surface problems before they affect your patient.
Does the lab track production consistency across batches?
Consistency matters most in repeat or multi-unit cases. For one DSO client operating across five U.S. locations, minor deviations between batches caused seating issues on implant models.
To solve this, we created a batch-locked color code and instituted a “cross-batch match review” in our post-curing QA step. Within two months, we were logging material lot numbers, printer groups, and curing timestamps on all trays. The client was able to trace and cross-check all remakes against batch ID, reducing complaint cycles significantly.
We now share a quarterly summary of delivery performance and root-cause stats for any remake. For multi-location clinics or procurement managers, this builds real visibility and confidence.
If a lab can’t tell you what’s been happening across their last 50 jobs, they won’t see the pattern before it becomes your problem.
What Evidence Can the Lab Provide to Support Their Claims?
Labs that back up their claims with verifiable evidence—case samples, certifications, and long-term performance summaries—show they don’t just promise results, they prove them.
In digital dentistry, trust comes from traceability. If a lab can’t show what they’ve done—and how they’ve measured it—you’re left taking their word at face value.

dental-lab-proof-of-quality
Can the lab share validated case samples involving 3D printing?
A lab should be able to show de-identified clinical cases, especially for 3D printed restorations or models. These might include:
- Before/after photos of long-span printed temps
- Model-to-restoration comparison charts
- Post-curing workflows and margin verification screenshots
Make sure these examples show the process, not just the outcome. This proves the lab isn’t “cherry-picking”—they’re standardizing.
Are there process certifications (e.g. ISO, internal QA protocols)?
Third-party certifications provide external accountability. Common frameworks include:
| Certification/Protocol | What It Ensures |
|---|---|
| ISO 13485 (Medical Devices) | End-to-end quality system for medical products (ISO 13485 certification details) |
| FDA Device Registration | Compliance with U.S. biocompatibility regulation |
| Internal QA Audit Log | Demonstrates how often the lab catches its own errors |
A well-managed lab should be able to explain what their certification covers, and how often they internally validate workflows—even outside audits.
How does the lab demonstrate long-term performance with key clients?
Data builds trust. One of our long-term clients—a regional group practice in Queensland—asked us to prove consistency after integrating 3D printed dies into their full-arch workflow.
We compiled six months of case-level reports: delivery dates, print methods, curing profiles, remake logs. The result? Less than 1.5% adjustment rate and a 4-hour average response time on any flagged case. We shared that in a performance dashboard they now review quarterly.
More importantly, the discussion helped shape a shared KPI: batch-level match rate across locations, now visible in their ordering portal.
If your lab can’t show long-term data or verified case performance, ask why not. Experience should be measurable.
What Questions Clarify the Lab’s Technical Readiness and Support Scope?
Digital tools mean little without responsive human support. Labs with the right hardware, but no systems to respond or coordinate, often cause delays when things don’t go as planned.
Clients should know—not just what machines the lab runs—but how well-prepared the team is to resolve problems, iterate quickly, and coordinate across roles.

dental-lab-technical-support-readiness
What 3D printers and software does the lab operate in-house?
Knowing what equipment is available tells you what’s realistically possible. Common commercial setups vary:
- Printer types: SLA (e.g. Form 3B+), DLP (e.g. Asiga Max), LCD-based platforms
- Software stack: Dental System (3Shape), Netfabb, exocad
- Material compatibility: Can they handle hybrid workflows or third-party resin tuning?
Labs that rely entirely on third-party printers or design teams may lack control when cases need rework or modifications. Ask if they validate and maintain their own print workflows
Who handles troubleshooting or client-side coordination if technical issues arise?
Support roles are often blurred. Some labs may have no dedicated digital lead—meaning any file issues go into a generic support queue.
Better labs typically assign:
- Design coordinator: first point of contact for scan or margin issues
- Print lead: manages machine validation, post-curing, resin lot tracking
- Client success liaison: helps schedule urgent reprints or escalations
Knowing who to call when something breaks avoids days of email loops. Ask if they have SLA-style support workflows—or rely on ad hoc email threads.
Is the lab able to support urgent or iterative prototyping requests?
One of our clients, a U.K.-based distributor, needed five prototype frameworks turned around in under 36 hours for an investor showcase. The clinic’s scan file arrived incomplete, and the window to reprint was tight.
Our team flagged the margin error within 90 minutes and coordinated a corrected scan through WhatsApp—outside formal hours. We split the build between two printers to save curing time and used overnight resin prep to meet shipping by the next evening.
That case wasn’t just about speed—it was about infrastructure and communication alignment. Since then, we’ve added a standing “rapid response” toggle in our intake form for all distributors needing iterative sampling.
Labs that treat urgency as a partner request—not an inconvenience—often make the difference between winning or losing a client’s trust.
Conclusion
Choosing a 3D printing–enabled dental lab isn’t just about technology—it’s about alignment. The right partner proves accuracy with data, certifies materials with traceability, and handles digital workflows with accountability. From turnaround metrics to urgent prototyping, a dependable lab should offer more than production—they offer visibility and control. As an overseas dental lab working closely with clinics, DSOs, and distributors, we believe technical readiness and communication clarity are as critical as the crowns we print. Evaluate proof, not promises—and look for those who treat your success as shared.