Verifying certifications and quality standards in a dental implant OEM lab is essential for ensuring safety, compliance, and long-term reliability. A qualified lab must show adherence to international standards, provide transparent documentation, and operate with a robust quality management system that safeguards both clinicians and patients.
Challenges: Many implant providers face risks such as counterfeit or expired certifications, inconsistent documentation, weak quality control, and labs failing to meet FDA or ISO requirements. These gaps often result in costly remakes, patient safety issues, and reputational damage.
Solutions & Outcomes: By verifying ISO 13485 and ISO 10993, cross-checking FDA registrations and 510(k) clearances, reviewing documented processes, and ensuring traceability with complaint-handling systems, providers can identify trustworthy OEM labs. The result is predictable implant performance, reduced clinical risk, regulatory compliance, and sustainable partnerships that support high-quality patient care.
Choosing an OEM lab with the right certifications is not just about compliance—it is the foundation of trust, risk reduction, and consistent implant success.
Verifying Essential Certifications
Choosing an OEM dental implant lab without verifying certifications is a major risk—certifications serve as the foundation of compliance, safety, and credibility. A qualified lab demonstrates its commitment to quality by holding recognized international and regional approvals that prove both technical capability and regulatory alignment.
Dental-Implant-OEM-Certifications
Key certifications every OEM dental lab must hold: ISO 13485 for medical device QMS
ISO 13485 is the global benchmark for medical device quality management systems. A certified lab proves it follows standardized processes for design, manufacturing, and risk management. For OEM partnerships, this ensures that implant restorations meet consistent clinical and regulatory requirements across markets.
Why FDA registration and 510(k) clearance matter in implant manufacturing
For labs producing implants or components for the U.S. market, FDA registration and 510(k) clearance are non-negotiable. They validate that devices are substantially equivalent to legally marketed products and are safe for patient use. Checking the FDA database ensures the lab’s claims are genuine.
The role of ISO 10993 for biocompatibility and sterilization standards
Implants must not only fit precisely but also be safe for long-term use in the body. ISO 10993 ensures that materials used in implant restorations have undergone biocompatibility testing, minimizing risks of toxicity, allergic reactions, or implant failure. This standard also supports sterilization validation.
How to cross-check certifications with public databases for authenticity
It is not enough for a lab to show certificates—you must verify them in official databases. For example, cross-checking ISO certificates with accredited registrars or searching the FDA’s 510(k) database can confirm authenticity. Reliable OEM labs will openly share registration numbers, expiration dates, and certifying bodies without hesitation.
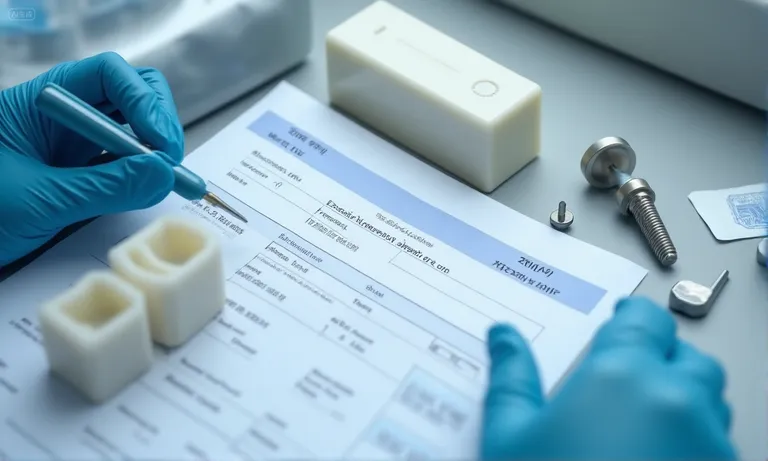
Checking Quality Standards and Documentation
Even when certifications are in place, the true measure of an OEM dental lab lies in its everyday quality control and documentation practices. Reliable partners provide full transparency into their material sources, process records, and QC protocols, ensuring that every implant product is traceable and meets required safety standards.

Dental-Lab-Quality-Documentation
Requesting material documentation and certificates of analysis
Every implant product begins with raw materials, and OEM labs must provide certificates of analysis (COA) for zirconia, titanium, or ceramic inputs. Reviewing these documents ensures biocompatibility and verifies that materials meet both ISO and FDA standards.
Reviewing manufacturing process records and maintenance logs
A high-quality OEM lab maintains detailed manufacturing process records. These include calibration data, machine maintenance logs, and batch production reports. Such records provide visibility into how consistently the lab can reproduce precise results.
Ensuring quality control protocols are documented and followed
A lab’s internal QC protocols—such as dimensional checks, surface finish inspection, and fatigue testing—must be well-documented and actively enforced. Without standardized QC, even a certified lab may deliver inconsistent outcomes.
Validating supply chain and external vendor compliance
Beyond internal processes, the reliability of implant restorations depends on the entire supply chain. OEM labs should validate that their external vendors and material suppliers also comply with ISO or CE requirements, ensuring end-to-end product integrity.
Assessing Operational Capabilities of the Lab
Certifications and documentation confirm compliance, but operational capabilities reveal whether an OEM dental lab can consistently deliver at scale. Evaluating the technical skillset, digital infrastructure, and case-handling capacity of a lab ensures they can meet both routine and complex implant demands without compromising quality or timelines.

Dental-Lab-Operational-Capabilities
Evaluating technician qualifications and implant experience
The expertise of technicians directly influences the quality of implant restorations. Look for labs where technicians are trained in implant-specific workflows, including abutment customization, full-arch restorations, and hybrid solutions. Experience across diverse implant systems ensures adaptability.
Reviewing CAD/CAM, scanner, and digital workflow readiness
A modern OEM lab must be fully integrated with CAD/CAM systems and digital scanning technology. This enables seamless file exchange, precise restorations, and compatibility with guided surgery workflows. Digital readiness is a hallmark of labs that support global implant brands.
Understanding case volume capacity and turnaround consistency
Scalability is key. A reliable OEM partner can handle high case volumes without compromising accuracy or timelines. Reviewing their average daily or monthly case output, alongside documented turnaround times, helps evaluate operational resilience.
How supplier evaluation impacts implant product reliability
Ultimately, the lab’s operational capabilities determine the predictability of outcomes. Weak infrastructure leads to bottlenecks, delays, and errors, while strong operational readiness results in consistent, high-quality implant products delivered on time.
Evaluating Quality Management Systems (QMS)
A dental implant OEM lab’s Quality Management System (QMS) is the backbone of reliable and repeatable outcomes. While certifications confirm compliance, the QMS reveals how effectively a lab enforces those standards in daily operations. A strong QMS provides confidence that every restoration—from single abutments to full-arch cases—meets strict clinical and regulatory requirements.

Dental-Lab-QMS-Compliance
Internal compliance policies and standard operating procedures
A robust lab QMS is built on well-documented standard operating procedures (SOPs) covering design, milling, finishing, sterilization, and packaging. Internal policies should reflect ISO 13485 and CE frameworks, ensuring uniformity across all processes.
Complaint handling and customer issue resolution systems
Effective QMS frameworks include structured systems for logging, investigating, and resolving customer complaints. Whether it’s a misfit abutment or esthetic concern, documented complaint-handling protocols show the lab’s commitment to accountability and continuous learning.
Traceability of materials and batch/lot numbers in implant production
Traceability is critical for medical devices. OEM labs must assign batch or lot numbers to materials and restorations, ensuring any product can be traced back to its source materials and manufacturing records. This not only supports recalls but also strengthens clinical confidence.
The importance of process validation for consistent outcomes
Beyond documentation, a strong QMS includes process validation. This means proving that CAD/CAM workflows, sintering protocols, or milling sequences consistently deliver expected results under real-world conditions. Process validation safeguards both repeatability and scalability.
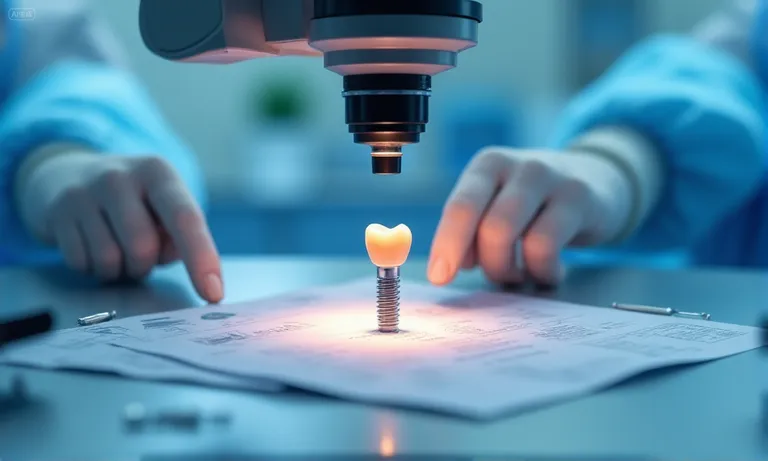
Implant-Specific Compliance and Safety Considerations
General certifications and QMS protocols establish a foundation, but implant-specific compliance and safety measures ensure that every component is safe, sterile, and clinically dependable. For OEM dental labs, overlooking these factors can lead to risks that directly impact patient outcomes. The following steps provide a clear roadmap for evaluation.
Image
ALT: Implant-Specific-Safety-Checks
Prompt: A dental implant component under microscopic inspection, surrounded by sterilization equipment, compliance checklists, and biocompatibility testing symbols.
Step 1. Material integrity and contamination prevention
Implant components must be produced and stored under strict contamination controls. Verify that the lab enforces cleanroom standards, sterilization protocols, and sealed packaging to prevent bacterial or particulate contamination.
Step 2. Ensuring biocompatibility through ASTM F981 and ISO 10993
Biocompatibility testing is not optional. OEM partners should comply with ASTM F981 and ISO 10993 standards, ensuring zirconia, titanium, and hybrid materials are safe for intraoral use and long-term tissue integration.
Step 3. FDA regulations on sterilization, implant design, and manufacturing
Labs producing implant components or accessories must demonstrate FDA compliance in sterilization validation, implant design approval, and risk management. Checking FDA registration and 510(k) submissions helps verify adherence to U.S. regulatory requirements.
Step 4. Reviewing clinical case outcomes and patient satisfaction
Beyond regulatory paperwork, request evidence of clinical performance—including case studies, patient satisfaction scores, or complication rates. Real-world outcomes confirm whether compliance translates into safe, reliable restorations.
Building Trust through Transparency and Continuous Improvement
While certifications and compliance confirm a lab’s technical capability, long-term OEM partnerships are built on trust, openness, and continuous improvement. A reliable dental implant OEM lab should demonstrate transparency in operations and commit to ongoing performance enhancement.
Dental-Lab-Transparency-Trust
| Transparency & Improvement Measure | Practical Role | Long-Term Impact |
|---|---|---|
| Clear documentation of materials, processes, and QC results | Builds clinician confidence by providing verifiable evidence | Reduces disputes and increases trust in product quality |
| Regular audits and third-party inspections | Ensures compliance is independently validated | Strengthens credibility and reassures global clients |
| Structured feedback and performance data review | Identifies recurring issues and tracks progress | Drives iterative improvement in implant product outcomes |
| Openness about costs, timelines, and challenges | Promotes honest collaboration and realistic planning | Reinforces mutual respect and sustainable partnerships |
By combining transparency with continuous refinement, labs not only improve day-to-day workflows but also establish themselves as trusted, long-term OEM partners. For clinicians, this means more predictable outcomes and greater confidence in scaling implant services.
Conclusion
Selecting the right OEM dental implant lab requires more than verifying certifications—it demands a clear understanding of safety, compliance, operational capacity, and transparency. A technically capable and trustworthy partner safeguards product quality, reduces risks, and ensures smoother clinical outcomes.
By working with an experienced overseas dental lab that values documentation, feedback, and continuous improvement, clinicians and businesses can build sustainable collaborations. The result is not only consistent implant quality but also a long-term partnership that supports clinical excellence, regulatory compliance, and growth.