Selecting a dental implant lab in China is not simply a matter of chasing the lowest price. For sustainable collaboration and predictable clinical outcomes, decision-makers need to assess a set of core dimensions that directly affect quality, efficiency, and trust.
Key evaluation factors include:
- Quality assurance systems — measurable remake rates, material traceability, and the use of genuine implant components.
- Digital workflow compatibility — support for standard file formats (e.g., STL, PLY) and clear real-time communication channels.
- Regulatory certifications — proof of ISO 13485, CE, and FDA compliance across both materials and processes.
- Logistics and turnaround reliability — realistic lead times and shipping coordination that do not compromise QA checks.
- Transparent pricing — understanding true cost structures and avoiding hidden expenses linked to remakes, urgency, or shipping.
- Collaboration models — clarity on OEM, ODM, or outsourcing options, and the lab’s flexibility in onboarding custom protocols.
- Risk indicators — potential gaps in communication, cultural alignment, or process transparency.
- Independent validation — third-party reviews, client feedback patterns, and small-scale pilots that confirm real-world performance.
Taken together, these criteria help buyers determine whether a partner lab can consistently deliver across case volume, complexity, and time. The goal is not only lower unit cost, but also higher predictability, reduced chairside adjustment, and durable clinical success.
How to assess dental lab quality for implant cases?
Successful implant work depends on proof of consistent outcomes, not promises. Before you choose a lab in China, look for hard signals: a traceable remake rate by category, a documented QC flow tied to device records, verified use of genuine components, and workmanship that stays stable as volumes grow. For governance baselines, confirm the lab aligns with ISO 13485.

Dental-implant-lab-qc-station
Why remake rate is a critical KPI for implant quality?
Remake rate shows process capability and where variation hides. Break it down by cause (fit, contact, occlusion, shade, screw seating) and by stage (pre-ship vs. post-seat) so you can act on it. Use a rolling 3–6-month trend with clear definitions of “remake” vs. “adjustment,” and track CAPA closure time by category.
- Split by category and stage for real signals.
- Assign an owner and due date for every CAPA.
- Share monthly trends with your team.
What does a structured QC process look like in Chinese labs?
A robust QC maps to medical-device recordkeeping: device master records and device history records that tie work orders, material lots, and acceptance criteria to each case. Ask how criteria are written, who signs off, and where records live. For reference language, see 21 CFR 820 — DMR and DHR. eCFR
How to ensure genuine implant parts are being used, not knockoffs?
Use identity you can verify.
- Keep packaging photos with UDI/DI in your case record; the FDA’s UDI system explains the identifiers.
- Random-sample items in AccessGUDID to confirm labeler and model; it’s the public device ID database.
- Align brands with your approved list; if a substitute is proposed, require written approval and updated IFU.
What signs show consistent craftsmanship at scale?
An independent two-op clinic in Brisbane piloted 20 posterior implant crowns over six weeks. Early cases showed inconsistent proximal contacts after sintering. We tightened the shared case form (contact targets, margin notes), added a second in-process check after staining, and locked a tooling set for these prescriptions. Adjustments fell from ~30% to ~10% by week four; no remakes in the final eight cases; chairside time per seat dropped ~12 minutes. As an overseas dental lab, we keep a single spec sheet per implant system so both teams speak the same shorthand.
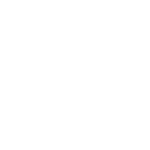
How to ensure smooth collaboration and digital workflow compatibility?
Smooth collaboration comes from two things: matching file ecosystems and shared, real-time communication habits. Before onboarding a Chinese implant lab, confirm open-format support (color where needed), test live response channels, and require simple, versioned workflow docs that your team can follow without extra calls.
Digital-workflow-implant-lab-collaboration
What file types and scanner outputs should your lab support (STL, PLY)?
For crowns and abutments, insist on open formats your team can audit and re-use. STL is universal but monochrome; PLY (and sometimes OBJ) retains color/texture for soft-tissue and scan-body detail; vendor-native DCM remains useful inside 3Shape. Check that your lab can ingest and export all three. See 3Shape’s notes on TRIOS exports (STL/DCM/PLY) and exocad’s supported meshes. For a quick primer on when STL vs PLY matters, review this file-format explainer from iDD: Understanding STL, PLY, OBJ. support.3shape.comwiki.exocad.comInstitute of Digital Dentistry
How to verify real-time communication capability for implant workflows?
Run a timed “day-zero” drill before the first live case.
- Open a shared chat and pick a single thread per case; confirm response SLA (<15 minutes during overlap hours).
- Ask the lab to screenshare a live design review and record decisions in-thread.
- Exchange a redline template for abutment parameters and shade notes; require same-day signoff.
- If PHI might appear, route through HIPAA-conscious channels and keep PHI out of subject lines. See ADA’s HIPAA FAQs for practical guardrails: HIPAA 20 Questions. 美国残疾人协会
A two-op clinic in Perth used this drill; average response time was 11 minutes and first-week clarifications dropped by half.
Why clear workflow documentation matters in remote collaboration?
Documentation prevents silent rework. Ask for a one-page “how we run implant cases” that includes: intake checklist (scan quality thresholds, scan-body IDs), file conventions (case ID, version tags), decision points (abutment parameter table), and a change log. Keep it versioned and linkable in your case thread. When teams rotate, this single page preserves context and cuts cycle chatter. As an overseas dental lab, we keep a living “case recipe” per implant system so your team sees the same defaults we manufacture against.
What certifications and compliance standards should a trusted lab meet?
Trust in a dental implant lab begins with proof of compliance, not verbal assurance. A qualified partner can show valid ISO certification, clear FDA/CE evidence for relevant devices and materials, and documented workflows aligned with those standards. These credentials should be current, independently verifiable, and mapped to both materials and processes.

Dental-lab-certification-display
What are the roles of ISO 13485, FDA, CE in dental implant production?
Each certification covers different ground. ISO 13485 demonstrates the lab’s quality management system is aligned with medical device manufacturing. FDA registration ensures any U.S.-bound components meet regulatory expectations under 21 CFR Part 820. CE marking applies to EU-bound devices, signifying conformity with European directives. Together, these show that both the workflow and the final device are monitored under recognized international frameworks. For reference, see ISO 13485 overview and the FDA’s Medical Device Quality System Regulation.
How to verify the scope and authenticity of a lab’s certifications?
Ask for a copy of certificates with registrar contact details and scope definitions. Cross-check ISO certificates on the registrar’s website; confirm FDA registration in the FDA Establishment Registration & Device Listing database; and search CE marks on the Notified Body’s site. Pay attention to scope wording: “manufacture of dental prosthetics” is not the same as “distribution.” Ensure the validity period and scope align with implant workflows. If details are vague, treat that as a red flag.
Why compliance across both material and workflow matters?
Compliance is not only about certificates on the wall—it extends to material sourcing, traceability, and workflow discipline. Materials like zirconia discs and implant components must come with certificates of analysis tied to batch numbers. Equally, the lab’s processes—design transfer, case record storage, CAPA handling—should reflect ISO 13485 structure. When materials and processes are both compliant, customers can defend outcomes in audits and reduce liability. As an overseas dental lab, we integrate certification records into case histories so clients always have evidence in hand.
What logistics efficiency and turnaround time should be expected from Chinese labs?
Turnaround depends on two clocks: production (CAD/CAM, sintering, QC) and transit (courier, customs, distance). For routine zirconia implant crowns, expect predictable lab cycles plus 2–5 business days of express shipping, with buffers for customs review and time-zone handoffs. Anchor your plan to service-level data from carriers and align cut-off times with your clinic’s schedule.
Implant-crown-logistics-timeline-china-to-us
What is the typical turnaround for zirconia implant crowns from China?
Plan production plus express transit. Most clinics see lab build (design → mill → sinter → stain → QC) within a defined window, then UPS Worldwide Express Saver (≈3–5 business days) or FedEx International Priority (≈1–3 business days, lane-dependent) for delivery to the U.S. For current service ranges, see UPS International services and FedEx International Priority. ups.comFedEx
How do labs manage shipping time zones, customs, and courier risk?
Use a “one-page lane plan” before the first case:
- Time-zone overlap:China (CST) is typically 15–16 hours ahead of U.S. Pacific Time; book design reviews during the daily overlap to protect cut-offs. A quick converter like WorldTimeBuddy keeps teams synced. Worldtime Buddy
- Customs hygiene:clean invoices (device description, material, HTS), declared value, consignee EIN, and consistent case IDs. Check current CBP Section 321 / de minimis guidance because thresholds and aggregation rules are actively evolving. U.S. Customs and Border Protection
- Courier selection:match parcel size and service level to risk; confirm pickup windows, Saturday options, and delivery SLAs on your lane with the carrier pages above.
What fast turnaround signals risk (e.g., skipped QC or outsourcing)?
If a lab quotes “next-day ship” on multi-unit implant zirconia, probe for skipped steps (no in-process checks, no post-stain verification) or unstable outsourcing. Ask to see the QC checklist timestamps tied to case IDs and courier manifests. A Sydney clinic we support tried a “rush lane” for eight posterior units: early loads returned in four days but required chairside adjustments on five of eight. After reinstating the second in-process check and locking a pickup at 18:00 CST, the same lane shipped in six days with only one minor adjustment. As a global dental lab, we prefer a transparent six-to-seven-day lane that preserves QC over an optimistic promise that erodes fit and trust.
What cost structure reflects real value vs. hidden risks?
Price alone never tells the full story. A reliable cost model for implant work balances direct line items with predictable hidden costs. Smart buyers look past the unit fee to total landed cost: case price + shipping + remake rate + urgent handling. Labs that make these drivers transparent create trust; labs that hide them create frustration and unpredictable ROI.

Dental-implant-lab-cost-breakdown
How to decode cost components in dental implant lab pricing?
Implant pricing typically has four visible categories—unit cost (crown, abutment, framework), design fees, finishing options (stain, layering), and shipping. Beyond that, check for courier surcharges, scan fees, or “handling” lines. A clear breakdown helps you compare labs on equal terms.
Why low price ≠ high ROI: balancing value and reliability
A unit fee 20% below market may look appealing, but if remake rates are high or shipping is inconsistent, chairside time and patient confidence suffer. ROI comes from fewer adjustments and predictable cycles, not the lowest headline price.
- Direct value: consistent fit reduces chairside time.
- Indirect value: fewer remakes protect schedule stability.
- Strategic value: trusted workflows reduce stress and patient churn.
Decision makers should weigh these against upfront discounts. Reliable partnerships often save more long-term.
What hidden costs (shipping, remake, urgency) often go unnoticed?
Consider a mid-size U.K. distributor that trialed two Chinese labs for 40 zirconia units. Lab A offered £10 less per crown but charged urgency surcharges and had a 15% remake rate. Lab B’s sticker price was higher, but remake was 5% and shipping included. Net cost per usable unit favored Lab B by ~12%.
Common blind spots:
- Shipping tiers (express vs. economy, fuel surcharges).
- Remake handling (who pays, courier covered or not).
- Rush orders (weekend or holiday markups).
As a Chinese dental lab working globally, we disclose these in pro forma quotes so buyers see total landed cost, not surprises.
What collaboration models are available for implant workflows?
Choosing the right collaboration model is less about labels and more about control, flexibility, and risk tolerance. Implant labs in China can support OEM, ODM, and outsourcing models, but each comes with different degrees of influence over design, delivery, and intellectual property. Understanding these differences helps procurement teams align the lab’s role with their own strategic needs.

Dental-lab-collaboration-models
How do OEM, ODM, and outsourcing models differ in control and risk?
- OEM (Original Equipment Manufacturing): You provide the design, the lab builds to spec. High control, but you carry most design risk.
- ODM (Original Design Manufacturing): The lab co-develops designs and provides technical input. Faster scaling, but less exclusivity.
- Outsourcing/Subcontracting: You offload specific cases or overflow to a partner lab. Flexible, but quality depends on alignment and oversight.
For a quick primer on these distinctions, see Investopedia — OEM vs ODM.
How flexible are Chinese labs in supporting custom design-to-delivery?
Flexibility often shows in file handling and prototyping support. A Canadian DSO ran a six-week pilot where the lab adapted its CAM nesting strategy to match the DSO’s abutment library, allowing in-house teams to reuse case files across multiple practices. This saved ~18% design time internally. As a global dental lab, we regularly adjust nesting, tool selection, or shading sequences to match client SOPs, provided changes are documented and repeatable.
What should a test-run or pilot collaboration process include?
Run a small, structured pilot before long-term commitment.
- Define scope: case types (single-unit, multi-unit), volume, and timeline.
- Set metrics: remake rate threshold, adjustment minutes, response time.
- Agree on workflow: file formats, approval steps, QC checkpoints.
- Review outcomes: compare results against metrics, document lessons, and refine.
Procurement teams should treat the pilot as a joint rehearsal; both sides invest in refining handoffs, not just ticking boxes.
What risks should be evaluated before outsourcing implant cases to China?
Most outsourcing failures trace back to mismatched expectations, opaque workflows, or weak verification. Reduce risk by aligning communication habits, demanding transparent records (materials, decisions, QC), and running due diligence with clear pass/fail gates before volume work begins. Treat risk management as a process, not a one-time checklist; frameworks like ISO 14971 (risk management for medical devices) help you structure it.

Implant-outsourcing-risk-checklist
What communication or cultural gaps could affect outcomes?
Risk rises when teams lack a single case thread, clear response SLAs, or shared vocabulary. Watch for soft language around “almost ready,” inconsistent time-stamp habits, or design notes buried in emails.
- Establish overlap-hour windows and <15-minute response SLAs for clarifications.
- Use one channel per case with versioned attachments.
- Maintain a “case glossary” for contacts, occlusion, emergence, and torque terms to prevent misinterpretation.
How to identify transparency issues in workflow or pricing?
Early warning signs often appear in documents. Use the table below to triage signals.
| Signal you see | What it may mean | Your move |
|---|---|---|
| No batch/lot on zirconia or screws | Weak traceability | Request COA + lot photos stored with the case ID |
| Design decisions missing from records | Risk of silent rework | Require a change log and signoffs in the case thread |
| “All-in” pricing with vague surcharges | Hidden landed cost | Ask for a cost sheet separating unit, shipping, rush, remake |
| Variable ship promises without cut-offs | Capacity/bottleneck gaps | Set fixed pickup windows and escalation paths |
| Refusal to share QC checklist | Steps being skipped | Pilot with mandatory pre-ship QC photos and timestamps |
What due diligence steps reduce supplier risk?
Run a short pilot with pass/fail criteria before scale.
- Validate legal and quality footing: certificate scope, registrar, validity; map to your device markets.
- Review materials: COA, UDI/DI photos, approved brands list.
- Test the workflow: send two typical cases and one edge case; measure remake rate, adjustment minutes, and response times.
- Audit records: confirm DHR ties case ID, lots, QC, and shipping data.
- Decide and document: if metrics pass, roll into a larger tranche; if not, close CAPA and retest.
As an overseas dental lab, we keep pilots small but rigorous, so both sides learn quickly with minimal patient risk.
What do other clinics and labs say about Chinese implant labs?
When procurement teams evaluate partners, independent voices often provide the most credible insights. Reviews, testimonials, and case feedback help validate claims about fit, finish, and long-term outcomes. The key is to look for patterns across multiple clinics and labs rather than focusing on a single story.

Dental-implant-lab-testimonials
Where to find real-world reviews or third-party testimonials?
Authentic feedback can be found through:
- Specialist forums like DentalTown or The Dental Lab Network, where clinicians exchange candid case experiences.
- Third-party platforms that capture broad client perspectives.
- Conferences or study clubs, where labs often share anonymized client case results.
- Peer introductions: many overseas dental labs facilitate reference calls with current clients when evaluating large-scale collaboration.
What feedback patterns relate to implant fit, finish, or success?
Recurring themes reported by clinics and DSOs often cluster around three dimensions:
| Feedback Category | Common Positive Signals | Red Flags to Watch |
|---|---|---|
| Fit | Minimal chairside adjustment, consistent occlusion | Frequent need for grinding, passive fit failures |
| Finish | Shade matching and polish praised | Over-polishing, surface roughness, mismatched translucency |
| Success | Low remake rates (<3%), stable long-term follow-up | High fracture rates, repeated screw loosening |
For instance, one U.S. clinic shared that after partnering with a Chinese lab for 18 months, their average adjustment time dropped by 22%. But another clinic reported variable translucency when rush orders bypassed normal QC — showing the need to filter both good and bad feedback through context.
How to interpret both positive and negative client feedback?
- Look for volume and pattern: one bad review is anecdotal; five with the same theme signal systemic issues.
- Weigh context: was the case a rush order, complex full-arch, or routine single crown?
- Confirm lab response: the most telling factor is whether the lab provides data, remakes, or process adjustments when issues arise.
As a global dental lab, we encourage potential clients to not only read external reviews but also to trial us with a small case set — bridging the “review gap” with their own firsthand experience.
Conclusion
Choosing a dental implant lab in China should feel disciplined, not risky. Prioritize partners who prove quality with measured remake rates, traceable QC, and genuine parts; who fit your digital stack and document workflows; who show valid ISO 13485 and market-specific compliance; and who publish realistic turnaround plans. Value comes from transparent total cost, not the lowest sticker price. Start with a small, metric-driven pilot and check third-party feedback for pattern, not anecdotes. As an overseas dental lab, our role is to collaborate—align files, timing, and records—so your team gets predictable seats and fewer surprises. That is how cross-border partnerships compound into trust.