In complex implant restorations, material selection is one of the most decisive factors for success. The choice of zirconia, titanium, or emerging digital materials directly influences restoration longevity, clinical stability, and patient satisfaction.
Key considerations include:
- Biocompatibility: Materials must integrate with bone and soft tissue to avoid complications.
- Strength and durability: The restoration should resist chewing forces over many years.
- Aesthetics: Natural shade and translucency, especially with zirconia, improve patient acceptance.
- Functionality: Precise fit and load-bearing capacity support long-term reliability.
As an overseas dental lab, Raytops ensures these standards by combining certified sourcing, strict quality control, and digital workflows. This collaborative approach allows clinics to select the right material confidently, balancing predictable outcomes with cost efficiency.
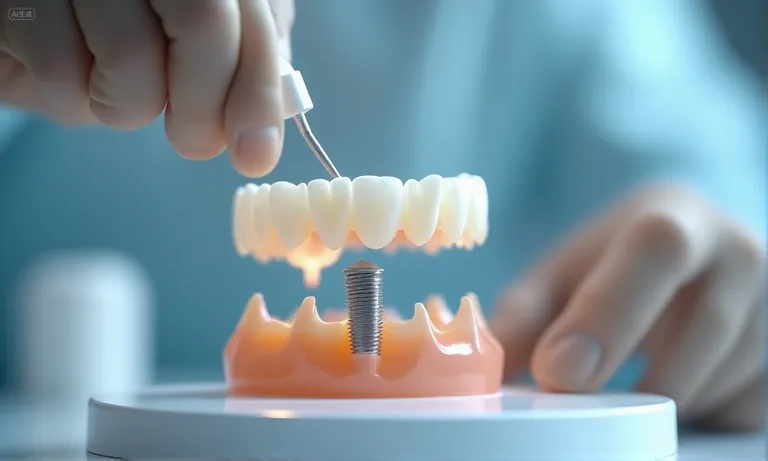
What Are the Key Factors to Consider When Selecting Materials for Complex Implant Restorations?
Selecting materials for complex implant restorations requires balancing biological safety, mechanical stability, and aesthetic expectations. Biocompatibility ensures integration with soft and hard tissue, durability determines whether the restoration withstands years of chewing force, and color matching influences how patients perceive treatment outcomes. From our perspective as an overseas dental lab, clients consistently prioritize these three dimensions when evaluating which material to use in advanced cases.

implant-material-selection-factors
Why Biocompatibility Is Crucial for Long-Term Success in Complex Restorations
Biocompatible materials such as titanium and high-translucent zirconia are proven to integrate well with bone and surrounding tissue. Lack of compatibility can trigger inflammation, prolonged healing, or even implant failure.
- Common biocompatible materials: titanium, zirconia, and medical-grade alloys.
- Risks of poor compatibility: peri-implantitis, patient discomfort, high remake rates.
- Labs often collaborate with clinics to validate whether selected materials meet ISO standards before large-scale use.
How Durability and Wear Resistance Impact the Lifespan of Implant Restorations
Restorations must handle years of chewing cycles and varied dietary forces. Materials with low wear resistance can fracture or cause opposing tooth damage.
- Zirconia offers excellent wear resistance but may be too rigid in some occlusal conditions.
- PFM (porcelain-fused-to-metal) remains popular for full-arch durability despite its aesthetic limitations.
- Clinical records show failures often correlate with underestimating mechanical demands rather than lab processing errors.
How Aesthetics and Color Matching Affect Patient Satisfaction
Even in complex implant cases, patient satisfaction often depends on appearance. Modern zirconia blocks and advanced staining techniques allow closer shade matching with adjacent teeth.
- Shade matching requires coordination between clinic photos, intraoral scans, and lab characterization techniques.
- In our collaborations, miscommunication of shade details is one of the most common remake triggers.
- Advanced labs now use digital shade scanners to reduce subjectivity and ensure consistency.
When clients assess biocompatibility, durability, and aesthetics together, they gain a more balanced view of material performance. As an overseas dental lab, we often see clinics weigh these factors differently depending on patient expectations, but ignoring any one dimension typically leads to higher remake risk or reduced trust. which align with what labs and clinics face in daily decision making.
How Do Different Materials Affect the Performance of Complex Implant Restorations?
Different materials affect implant restorations by determining strength, longevity, and adaptability to complex anatomical cases. Zirconia and titanium dominate high-strength applications, porcelain-fused-to-metal (PFM) remains reliable for full-arch frameworks, and 3D-printed polymers and resins are now enabling highly customized precision fits. Each choice reflects a balance between mechanical properties, aesthetics, and workflow efficiency.

implant-materials-performance-comparison
How Zirconia and Titanium Compare in Terms of Strength and Application for Complex Cases
Zirconia and titanium are both trusted in complex implant scenarios, but they serve different roles.
| Property | Zirconia | Titanium |
|---|---|---|
| Strength | High compressive strength, rigid | High tensile strength, flexible |
| Biocompatibility | Excellent with soft tissue aesthetics | Gold standard for osseointegration |
| Aesthetic quality | Tooth-colored, natural look | Metallic, requires veneering |
| Application | Suprastructures, visible restorations | Implants, abutments, load-bearing zones |
| Clinics often pair titanium for implant fixtures with zirconia for visible restorations, leveraging both benefits. |
The Benefits of Porcelain-Fused-to-Metal (PFM) for Full-Arch Restorations
PFM remains a mainstay in cases requiring durability across multiple units.
- Strong bond between metal substructure and porcelain veneer.
- Cost-effective compared to full-zirconia arches.
- Proven performance in long-term follow-ups, especially when aesthetic demands are moderate.
Despite newer options, labs still see PFM requested by clinics managing full-arch loads where budget and reliability are equally critical.
Why 3D-Printed Materials Are Ideal for Custom Fit and Precision
3D printing has reshaped complex case handling by allowing customized design and faster prototyping.
- Enables accurate try-ins and reduced chairside adjustments.
- Supports surgical guides, temporary restorations, and test frameworks.
- Reduces turnaround time by integrating directly with digital scans.
From our experience as an overseas dental lab, clinics often value 3D-printed components to preview occlusion and fit before finalizing zirconia or titanium restorations.
Labs and clinics that combine zirconia, titanium, PFM, and 3D-printed solutions can tailor their approach to each case’s mechanical and aesthetic demands. External comparisons such as NCBI’s review on implant material performance reinforce how different materials complement rather than replace one another in advanced cases.
Why Material Compatibility Is Critical for Complex Implant Restorations?
Material compatibility is critical because mismatched surfaces, coatings, or alloys can disrupt osseointegration, extend healing time, and lead to premature implant failures. When the implant fixture, abutment, and restoration material work in harmony, the result is predictable stability. But when compatibility is overlooked, both clinical outcomes and patient trust suffer.
Image
ALT: implant-material-compatibility-check
Prompt: A highly realistic, ultra-detailed, professional-quality photo captured in a clean, well-lit environment. Materials must be photorealistic, and rendered with DSLR-level clarity. Lighting should be soft daylight or studio white light, avoiding cold or bluish clinical tones. A close-up of a dental technician fitting a zirconia abutment onto a titanium implant placed in a bone model, checking compatibility and stability at the interface.
How Material Compatibility Affects Osseointegration and Healing Time
When materials are compatible, the bone forms a strong interface around the implant surface and healing progresses normally.
- Titanium with proven surface treatments shows high osseointegration rates.
- Zirconia abutments paired with titanium fixtures reduce soft tissue irritation while maintaining strength.
- Poor compatibility, such as mixing alloys with different corrosion profiles, can trigger micro-gaps and longer healing phases.
The Impact of Material Mismatch on Implant Failure and Complications
Mismatched components increase mechanical and biological risks.
- Different thermal expansion rates between metal and ceramic can create cracks.
- Electrochemical reactions between dissimilar alloys may accelerate corrosion.
- Clinical failures often appear as screw loosening, peri-implantitis, or restoration fractures.
Labs frequently identify remakes linked to overlooked compatibility checks in early planning stages.
How Consistent Material Quality Ensures Long-Term Implant Success
Even with the right combination, quality variation between material batches can undermine outcomes.
- Certified suppliers provide traceability and compliance with ISO and FDA standards.
- Overseas dental labs often coordinate with clinics to document lot numbers for implants and restorative components.
- Consistency lowers remake risk and reassures patients that results will remain stable over time.
Ignoring compatibility often means higher costs and more remakes later. From our collaborations as an overseas dental lab, we’ve seen how clinics that standardize implant–abutment–restoration systems enjoy smoother workflows and fewer complications. A helpful resource is the Journal of Prosthodontics study on implant component compatibility, which highlights how mismatches directly impact clinical outcomes.
How Does Raytops Ensure High-Quality Material Selection for Complex Implant Restorations?
Raytops ensures high-quality material selection by combining strict sourcing controls, advanced material integration, and a fully digital workflow. This structured approach minimizes remake risks and gives overseas partners confidence that restorations will meet both clinical and aesthetic expectations without compromise.
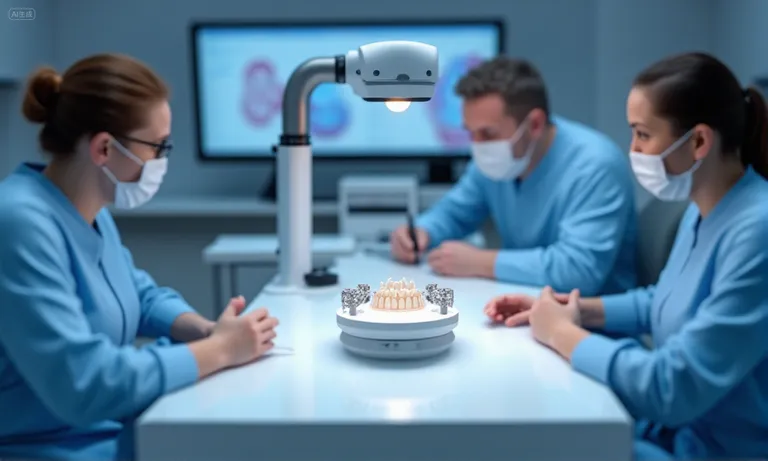
raytops-dental-lab-material-quality-control
The Role of Quality Control in Sourcing and Testing Implant Materials
Raytops collaborates only with suppliers that provide certified zirconia, titanium, and alloy products meeting ISO and FDA standards.
- Each batch undergoes hardness and stress tests before entering production.
- Digital scanning is used to verify density and purity of zirconia blocks.
- Titanium components are checked for micro-defects that could weaken osseointegration.
This layered control system ensures only consistent, clinically safe materials are used.
How Raytops Integrates Advanced Materials Like Zirconia and Titanium into Custom Solutions
Different cases demand different material combinations, and Raytops adapts by integrating them into custom workflows.
- Zirconia is selected for visible restorations requiring both strength and aesthetics.
- Titanium is applied for abutments and load-bearing areas, ensuring structural stability.
- Hybrid solutions, such as zirconia veneered over titanium frameworks, are created when full-arch durability and esthetics must be balanced.
Clients value this adaptability because it prevents material mismatch and aligns with case-specific needs.
Why Raytops’ Digital Workflow Ensures Precise Material Selection and Fit
Digital workflows reduce human error and create predictable outcomes.
- Incoming digital scans are aligned with CAD libraries containing certified material data.
- Software simulations flag potential weak points or design mismatches before milling.
- CAM equipment is calibrated to match the specific material properties of zirconia, titanium, or hybrid structures.
This step-by-step system eliminates guesswork and delivers restorations that fit accurately the first time.
Raytops’ process shows how an overseas dental lab can use discipline and digital precision to reduce remake rates and build trust with long-term clients. A reference such as DE’s Business Lab: Digital workflows for maximum efficiency (Dental Economics) reflects the same trend: when labs embed quality checks and digital systems, results improve across the board.
What Are the Cost Considerations for Material Selection in Complex Implant Restorations?
Material selection directly affects the overall cost of complex implant restorations, not only in upfront pricing but also in long-term maintenance and remake risks. Choosing the right material is less about finding the cheapest option and more about balancing performance, patient satisfaction, and financial sustainability.

Image
ALT: implant-materials-cost-comparison
Prompt: A highly realistic, ultra-detailed, professional-quality photo captured in a clean, well-lit environment. Materials must be photorealistic, and rendered with DSLR-level clarity. Lighting should be soft daylight or studio white light, avoiding cold or bluish clinical tones. A dental procurement manager reviewing cost sheets on a desk with samples of zirconia discs, titanium abutments, and a PFM framework arranged side by side.
How Material Choice Impacts the Overall Cost of Complex Restorations
Each material carries unique cost implications for clinics and labs.
- Zirconia restorations require advanced milling but offer lower long-term remake costs.
- Titanium remains cost-effective for abutments but may need veneering for aesthetics.
- PFM is less expensive initially but can result in more remakes due to chipping or color mismatch.
Ignoring long-term impact often results in hidden costs beyond the initial invoice.
Understanding Cost-Effective Material Options Without Compromising Quality
Clinics and labs often evaluate materials based on value rather than lowest cost.
| Material | Initial Cost | Long-Term Risk | Best Use Case |
|---|---|---|---|
| Zirconia | High | Low (few remakes) | Visible restorations, complex bridges |
| Titanium | Moderate | Very low | Implants, abutments, load-bearing areas |
| PFM | Moderate | Moderate to high | Full-arch restorations with lower esthetic demand |
| 3D-printed | Low | Variable | Temporary restorations, try-ins, surgical guides |
| This balance helps procurement teams optimize budgets without sacrificing patient outcomes. |
The Long-Term Value of Investing in High-Quality Materials for Complex Cases
Higher-quality materials often save costs by reducing remakes, improving patient satisfaction, and shortening chairside time.
- Clinics using consistent zirconia sources report fewer shade mismatch remakes.
- Abutments made from certified titanium lower complication-related costs.
- Overseas dental labs like Raytops emphasize this long-term value during collaboration, highlighting how stable sourcing builds trust with both clients and patients.
Balancing material costs is ultimately about total case value, not just price tags. Industry resources like the cost-effectiveness analysis of implant-retained prostheses (implant-retained overdentures) confirm that long-term outcomes often justify initial investment in higher-grade materials.
Conclusion
Choosing the right material for complex implant restorations is not just a technical step—it is a strategic decision that shapes long-term clinical success, patient satisfaction, and cost efficiency. Biocompatibility, durability, aesthetics, compatibility, and value all play interconnected roles in ensuring predictable outcomes.
From our perspective as an overseas dental lab, we have seen that clients who prioritize both material quality and workflow integration face fewer remakes, smoother collaboration, and stronger patient trust. By combining certified sourcing, digital workflows, and careful cost-value evaluation, labs and clinics together can achieve restorations that are not only functional but lasting investments.